Most people think of loperamide as just another drugstore remedy for a bad stomach. You grab a bottle of Imodium A-D, take two pills, and within a few hours, the cramps and urgency fade. It’s safe, it’s legal, and it’s right there on the shelf next to painkillers and antacids. But what if that little blue bottle is hiding something far more dangerous than a case of food poisoning?
Since 2010, a quiet but deadly trend has emerged: people are swallowing dozens, sometimes hundreds, of loperamide pills-not to stop diarrhea, but to chase opioid-like highs or numb the agony of withdrawal. The FDA first sounded the alarm in 2016, and since then, emergency rooms have seen a steady rise in cases of people collapsing from heart rhythms so chaotic, they can kill in minutes. This isn’t a myth. It’s happening right now, and most people have no idea.
How Loperamide Works-And Why It’s Being Misused
Loperamide is an opioid, but not the kind you think of. Unlike heroin or oxycodone, it was designed to stay in your gut. At normal doses-1 or 2 pills, no more than 8 mg a day-it binds to opioid receptors in your intestines. That slows down bowel movements, which is exactly what you want when you’re running to the bathroom every ten minutes. The body’s natural defense keeps it from crossing into the brain: a protein called P-glycoprotein acts like a bouncer, kicking loperamide out before it can reach the central nervous system.
But when someone takes 50, 100, even 400 mg in a single day-equivalent to 25 to 200 regular pills-that bouncer gets overwhelmed. The excess loperamide slips through. It reaches the brain. And suddenly, it starts acting like a weak version of methadone or heroin: dulling pain, calming anxiety, reducing withdrawal symptoms. For someone trying to quit opioids, it’s tempting. It’s legal. It’s cheap. And it’s easy to get.
Here’s the catch: you have to take a terrifying amount to feel anything. And that’s where the danger explodes.
The Heart Doesn’t Care About Your Intentions
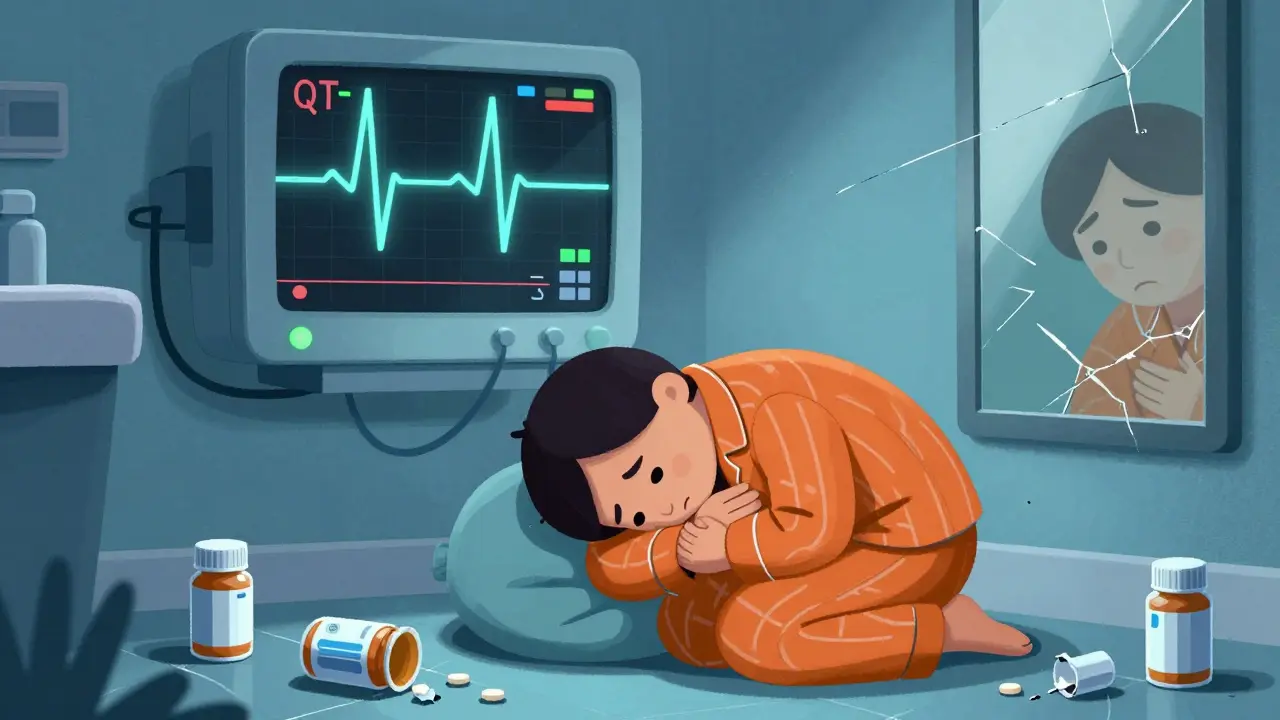
At therapeutic doses, loperamide is harmless to the heart. At abusive doses, it becomes a silent killer. The drug blocks potassium channels in heart cells-the same channels targeted by drugs like quinidine and sotalol, which are strictly controlled because they can trigger deadly arrhythmias. When loperamide does this, it stretches out the heart’s electrical cycle. On an ECG, that shows up as a prolonged QT interval. If it gets bad enough, the heart starts quivering instead of pumping. That’s torsades de pointes: a type of ventricular tachycardia that can turn into cardiac arrest within seconds.
The FDA reviewed 48 serious cases of loperamide-related heart events. More than half happened after 2010. In one case, a 32-year-old man with opioid addiction was taking 80 mg a day-20 times the maximum recommended dose. He ended up in the ER with polymorphic ventricular tachycardia, a prolonged QTc of 560 ms, and temporary heart failure. He survived. Many don’t.
Between 2011 and 2020, at least 17 deaths were directly tied to loperamide overdose. And those are just the ones that got reported. Many more likely went uncounted, misdiagnosed as heart attacks or sudden cardiac death with no explanation.
Warning Signs No One Talks About
If someone you know is abusing loperamide, the signs aren’t always obvious. They won’t be slurring their words or nodding off like someone on heroin. Instead, look for these red flags:
- Buying multiple bottles of Imodium at once-sometimes 10 or more in a single trip
- Using loperamide in combination with other drugs like diphenhydramine (Benadryl), cimetidine (Tagamet), or quinidine to boost absorption
- Complaining of chest pain, palpitations, dizziness, or fainting spells, especially after taking more than 4 pills
- Extreme constipation, bloating, or a feeling that their intestines have shut down
- Sudden changes in behavior: isolating, hiding medications, becoming defensive when asked about their health
These aren’t just signs of a bad habit. They’re signs of a medical emergency waiting to happen.
Why People Turn to Loperamide Instead of Real Treatment
Many who abuse loperamide aren’t chasing a high-they’re trying to survive withdrawal. Opioid withdrawal is brutal: muscle aches, nausea, vomiting, diarrhea, anxiety, insomnia. It’s no wonder someone desperate would look for a quick fix. But here’s the truth: loperamide isn’t a substitute for treatment. It’s a trap.
Medications like buprenorphine and methadone are proven, medically supervised tools for managing opioid dependence. They’re dosed carefully, monitored for side effects, and paired with counseling. Loperamide has none of that. No doctor. No safety net. Just a person alone in a bathroom, swallowing pills until their heart starts to fail.
A 2018 study in the Journal of Addiction Medicine found that 15.3% of people with opioid use disorder had tried loperamide to manage withdrawal. That’s more than 1 in 7. And for every person who gets help, dozens more are doing this in secret.
What’s Being Done-and Why It’s Not Enough
After the FDA warning in 2016, the industry made some changes. Some brands switched to single-dose blister packs for bottles containing more than 45 mg. That makes it harder to swallow 20 pills at once. Sales dropped 12% between 2016 and 2020. But people adapted. They buy online. They order bulk packs from overseas. They split pills. They mix loperamide with other substances to make it work faster.
And here’s the worst part: standard drug tests don’t detect loperamide. Emergency rooms often miss it. A patient comes in with cardiac arrest. Doctors check for cocaine, heroin, alcohol. They don’t think of Imodium. By the time they do, it’s too late.
The American College of Medical Toxicology now recommends that any patient with unexplained QT prolongation and a history of opioid use be tested for loperamide. But that’s not standard practice everywhere. Many clinics still don’t know to ask.

What to Do If You or Someone You Know Is Using Loperamide Abusively
If you’re taking more than 8 mg a day, stop. Now. Don’t wait for symptoms. Don’t wait for someone to notice. The damage can happen fast-and it’s often irreversible.
If you’re helping someone else:
- Don’t confront them with judgment. Shame drives people deeper into secrecy.
- Ask open questions: “Have you been taking more than the label says?” “Do you ever feel your heart racing after taking it?”
- Encourage them to see a doctor-or a toxicologist-if they’re having chest pain, dizziness, or irregular heartbeat.
- Help them find real treatment. SAMHSA’s National Helpline (1-800-662-HELP) connects people to opioid treatment programs. Buprenorphine can be prescribed by trained doctors, even in rural areas.
- Keep naloxone on hand. While it doesn’t reverse loperamide’s cardiac effects, it may help if opioids are also involved.
There’s no shame in needing help. But there’s huge risk in thinking you can outsmart a drug that’s designed to kill you if you take too much.
Final Reality Check
Loperamide isn’t a gateway drug. It’s a trapdoor. It looks harmless. It’s sold next to cough syrup. It’s been on shelves for nearly 50 years. But the moment someone crosses the line from 8 mg to 80 mg, they’re playing Russian roulette with their heart.
The people abusing it aren’t criminals. They’re not addicts looking for a thrill. They’re someone’s son, daughter, brother, or friend-trying to get through the worst days of their life without professional help. And they’re doing it with a drug that doesn’t care how desperate they are.
If you’ve ever thought, "I’ll just take a few extra pills to feel better," stop. That’s not self-care. That’s self-harm. And it’s more common than you think.
There are better ways. There are people who can help. But you have to reach out before your heart gives out.
Can you get addicted to loperamide?
Yes, though not in the same way as heroin or oxycodone. Loperamide doesn’t produce strong euphoria, so physical dependence is less common. But people develop psychological dependence, especially those using it to manage opioid withdrawal. They feel they can’t function without it, leading to compulsive use at dangerous doses.
How much loperamide is too much?
The maximum recommended daily dose for over-the-counter use is 8 mg. Anything above that increases risk. Abuse typically starts at 20-30 mg per day and can go as high as 400 mg. Even 12-16 mg can cause dangerous heart rhythm changes in sensitive individuals. There’s no safe "extra" dose.
Does loperamide show up on drug tests?
No, standard urine drug screens don’t detect loperamide. It’s not included in panels for opioids, benzodiazepines, or amphetamines. Specialized toxicology tests are needed, which most hospitals don’t run unless loperamide abuse is suspected. This often leads to misdiagnosis.
Can naloxone reverse loperamide overdose?
Naloxone may reverse some of the central opioid effects of loperamide, like sedation or respiratory depression, but it does nothing for the cardiac toxicity-the main cause of death. QT prolongation, torsades de pointes, and heart arrest require immediate medical intervention: IV magnesium, pacing, or defibrillation. Naloxone alone won’t save you.
Is loperamide still safe to use for diarrhea?
Yes, when used as directed. For occasional diarrhea, 2 mg initially, then 1 mg after each loose stool (up to 8 mg total per day), loperamide is safe and effective. The risk comes from misuse-taking more than directed, using it daily, or combining it with other substances. Don’t use it for more than 48 hours without seeing a doctor.
What should I do if I suspect someone is abusing loperamide?
Don’t ignore it. If someone is taking more than the label says, especially if they have a history of opioid use or are showing signs of heart problems (chest pain, fainting, irregular heartbeat), encourage them to see a doctor immediately. Offer to go with them. If they’re in crisis, call emergency services. Loperamide toxicity can kill within hours.
Next Steps for Safer Use
If you use loperamide regularly for chronic diarrhea, talk to your doctor. There are better long-term solutions-diet changes, probiotics, prescription medications like eluxadoline-that don’t carry cardiac risks.
If you’re using it to manage withdrawal, please reach out to a treatment center. You don’t have to do this alone. Medication-assisted treatment works. It’s safe. And it saves lives.
And if you’ve ever thought loperamide was harmless because it’s over-the-counter-remember this: just because something is easy to buy doesn’t mean it’s safe to abuse.

