When you’re pregnant, even a simple headache or stuffy nose can feel like a crisis. You want relief-fast. But you’re also terrified of doing something that might hurt your baby. That’s why so many women reach for an OTC medicine without thinking twice. And that’s exactly where the danger lies.
Not All OTC Medications Are Created Equal
You might assume that if a drug is sold over the counter, it’s safe. That’s a dangerous myth. The truth? Some OTC medications are fine. Others can raise your risk of miscarriage, birth defects, or long-term developmental issues. And the risks change depending on which trimester you’re in.Acetaminophen (Tylenol) is still the go-to for pain and fever during pregnancy. It’s been studied more than any other OTC drug in pregnant women. The standard safe dose is 650-1,000 mg every 4-6 hours, with no more than 4,000 mg in 24 hours. Even in the first trimester, when the baby’s organs are forming, acetaminophen is considered the safest option-if used as directed.
But here’s the catch: new research is raising questions. A large study tracking 50,000 pregnancies is currently looking at whether long-term or high-dose acetaminophen use might be linked to attention or behavioral issues in children. The findings aren’t final yet, but they’re enough to make experts urge caution. Don’t take it longer than you need to. Don’t take more than you need to. And never use it as a daily crutch.
NSAIDs: Avoid After Week 20-And Be Careful Earlier
Ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin belong to a class called NSAIDs. These are common, cheap, and effective. But they’re not safe during pregnancy, especially later on.The FDA issued a strong warning in 2020: NSAIDs can cause serious kidney problems in the developing baby after 20 weeks. That means reduced amniotic fluid, which can lead to lung underdevelopment and limb contractures. In rare cases, it can even cause heart failure.
But the risks don’t stop there. Studies show that using NSAIDs in the first trimester may increase the chance of miscarriage by up to 60%. That’s not a small number. Even a single dose of ibuprofen during early pregnancy can be risky if you’re already at risk for pregnancy loss.
Bottom line: Skip NSAIDs entirely unless your doctor says otherwise. And if you’ve already taken some, don’t panic-but do mention it at your next appointment.
Decongestants: The Hidden Danger
Pseudoephedrine (Sudafed) is a common decongestant. It’s in a lot of cold and sinus medicines. But if you take it in the first trimester, you’re increasing the risk of a rare but serious birth defect called gastroschisis-where the baby’s intestines develop outside the abdomen.Research shows this risk goes up by more than double. That’s why most doctors tell pregnant women to avoid pseudoephedrine in the first 12 weeks. Even if you’re just taking it for three days, it’s not worth the gamble.
And here’s another trap: many cold medicines combine decongestants with pain relievers or cough suppressants. So if you grab a bottle labeled “Cold & Flu,” you might be getting pseudoephedrine without even knowing it. Always read the active ingredients. Look for “phenylephrine” too-it’s another decongestant with limited safety data in pregnancy.
Antihistamines: Which Ones Are Safe?
Allergies don’t take a break during pregnancy. But not all antihistamines are equal.Loratadine (Claritin) and cetirizine (Zyrtec) are considered safe throughout pregnancy. Fexofenadine (Allegra) is now also included in this group, based on a 2022 study of over 12,000 pregnancies. These are second-generation antihistamines-they don’t cause drowsiness and have the best safety record.
Chlorpheniramine (found in some older allergy meds) is also considered acceptable, though it can make you sleepy. But diphenhydramine (Benadryl)? Use it sparingly. It’s not proven to cause birth defects, but it crosses the placenta easily and can affect fetal heart rate. Plus, it’s often in nighttime cold remedies. If you’re taking it to sleep, talk to your doctor about safer alternatives.
Heartburn and Diarrhea: Simple Fixes, Big Mistakes
Heartburn is almost guaranteed during pregnancy. Tums (calcium carbonate) is a great first choice. You can take up to 2,000 mg a day safely. Maalox, Mylanta, and Pepcid AC (famotidine) are also fine.But don’t go overboard. Too much calcium can cause constipation or kidney stones. And never use antacids with aluminum unless your doctor says so-they can build up in your system.
For diarrhea, loperamide (Imodium) is okay if you don’t have a fever and you follow the package instructions. But if your diarrhea lasts more than two days, call your provider. It could be something like listeria or a stomach virus that needs treatment.
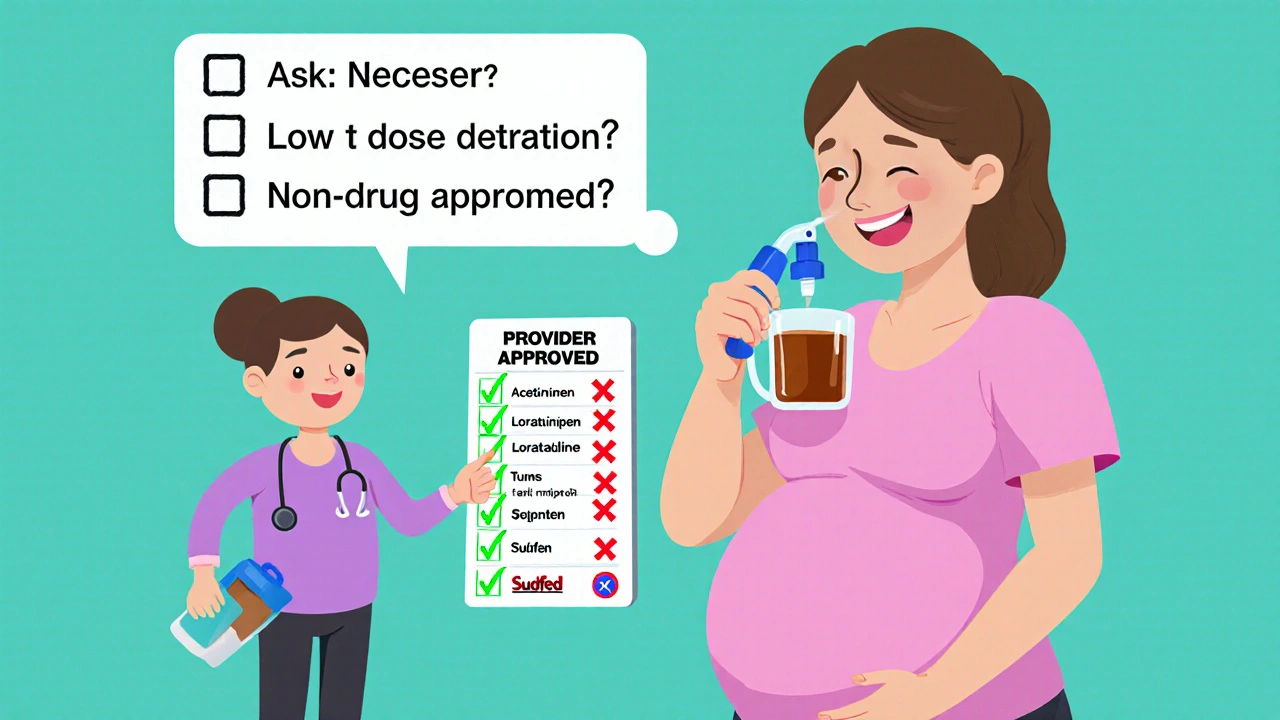
What You Should Ask Before Taking Anything
The real question isn’t “Is this safe?” The real question is: What do I need to ask before I take it?Here are the five questions every pregnant woman should ask before reaching for an OTC bottle:
- Is this medication absolutely necessary? Can I manage this with rest, hydration, saltwater gargles, or a humidifier?
- What’s the lowest dose that will work? Don’t take two pills if one will do. Start low.
- How long will I need it? A day or two? Fine. A week? Talk to your doctor.
- Are there non-drug options? For headaches: cold compress, massage, deep breathing. For congestion: saline spray, steam, nasal strips. For heartburn: eat smaller meals, avoid spicy food, don’t lie down after eating.
- Has my provider approved this exact product? Brand names matter. “Plain Robitussin” (just dextromethorphan) is safe. “Robitussin Multi-Symptom” contains phenylephrine and acetaminophen-avoid it.
The Biggest Mistake: Assuming “Natural” Means Safe
Herbal teas, ginger supplements, essential oils, and “natural” cold remedies are everywhere. But “natural” doesn’t mean safe. Some herbs like black cohosh, goldenseal, and pennyroyal can trigger contractions or miscarriage. Even chamomile and peppermint tea in large amounts can affect hormone levels.There’s almost no regulation of herbal products. They don’t have to prove safety during pregnancy. So if you’re thinking about a supplement, ask your provider first-even if it’s on the shelf at the health food store.

What to Do If You’ve Already Taken Something
If you took ibuprofen last week for a headache? Don’t panic. One dose is unlikely to cause harm. But don’t ignore it either. Write it down: what you took, how much, when, and why.Bring that list to your next prenatal visit. Most doctors will ask you about OTC use anyway. But if you’re worried, call your provider sooner. They can check for signs of complications and give you peace of mind.
And if you’re planning to get pregnant? Start this conversation now. Talk to your doctor about your current medications-even if they’re just for allergies, migraines, or acid reflux. Getting your meds sorted before conception is the best way to protect your future baby.
Keep a Medication Log
The CDC recommends keeping a full list of everything you take during pregnancy: prescription drugs, OTC meds, vitamins, herbs, and even topical creams. Include brand names, dosages, and how often you take them.Many women don’t realize that even a daily multivitamin can interact with other supplements. And some cough syrups still contain alcohol-even if they say “alcohol-free.” Always check the inactive ingredients.
At your first prenatal visit, bring this list. It’s one of the most helpful things you can do. It helps your provider spot risks you didn’t even know about.
Final Thought: You’re Not Alone
You’re not careless for wanting to feel better. You’re human. But you’re also carrying a life that can’t speak for itself. That’s why asking the right questions matters more than ever.There’s no perfect answer. No medication is 100% risk-free. But there are clear, evidence-based choices that minimize risk. Stick to acetaminophen. Avoid NSAIDs after week 20. Skip decongestants early on. Stick to proven antihistamines. And always, always check with your provider before taking anything new-even if it’s on the shelf next to the gum and mints.
Your baby’s health isn’t about avoiding all risk. It’s about making smart, informed choices. And that starts with asking the right questions before you swallow that pill.
Is Tylenol really safe during pregnancy?
Yes, acetaminophen (Tylenol) is currently considered the safest pain reliever during pregnancy when used as directed. The standard dose is 650-1,000 mg every 4-6 hours, not exceeding 4,000 mg in 24 hours. It’s safe in all trimesters, but long-term or high-dose use is under study for potential links to neurodevelopmental effects. Always use the lowest dose for the shortest time needed.
Can I take Advil or ibuprofen while pregnant?
No, avoid ibuprofen and other NSAIDs after 20 weeks of pregnancy. The FDA warns they can cause serious kidney problems in the fetus and reduce amniotic fluid. Even before 20 weeks, studies link NSAID use to a higher risk of miscarriage. If you need pain relief, choose acetaminophen instead.
Is Sudafed safe during pregnancy?
Pseudoephedrine (Sudafed) should be avoided in the first trimester due to a higher risk of gastroschisis, a rare abdominal wall defect. After the first trimester, it may be used briefly under medical supervision, but safer alternatives like saline sprays or humidifiers are preferred. Always check labels-many cold medicines contain pseudoephedrine without making it obvious.
What cold medicines are safe during pregnancy?
Safe options include plain Robitussin (dextromethorphan only), loratadine (Claritin), cetirizine (Zyrtec), acetaminophen for pain/fever, and saline nasal sprays. Avoid multi-symptom products like “Cold & Flu” or “Day/Night” formulas-they often contain unsafe ingredients like phenylephrine, pseudoephedrine, or NSAIDs. Always read the active ingredients list.
Are herbal remedies safe during pregnancy?
No, most herbal remedies are not proven safe during pregnancy. Products like black cohosh, goldenseal, and pennyroyal can trigger contractions or miscarriage. Even common herbs like chamomile or peppermint in large amounts may affect hormones. There’s little regulation or research on herbal products for pregnant women. Always talk to your provider before using any supplement or tea.
What should I do if I took something unsafe by accident?
Don’t panic. A single, occasional dose of an unsafe medication is unlikely to cause harm. But write down what you took, how much, and when. Bring that information to your next prenatal visit. Your provider can assess your risk and may recommend monitoring if needed. It’s better to be honest and informed than to hide it out of fear.
Can I take antacids like Tums while pregnant?
Yes, calcium carbonate (Tums) is safe and often recommended for heartburn during pregnancy. You can take up to 2,000 mg per day. Other safe options include Mylanta, Maalox, and Pepcid AC (famotidine). Avoid antacids with aluminum unless your doctor approves them, and don’t use them daily without checking in with your provider.


Chris Vere
It's interesting how we treat OTC meds like they're harmless snacks when they're not. We forget that even water can be toxic in excess. The real issue isn't the medication-it's the mindset that anything available without a prescription is automatically safe. Pregnancy doesn't make you irrational. It makes you responsible. And responsibility means reading labels, not just trusting the bottle.
It's not about fear. It's about awareness.
November 21, 2025 AT 09:48
Pravin Manani
From a pharmacovigilance standpoint, the risk stratification outlined here is clinically robust. Acetaminophen remains the first-line analgesic in pregnancy due to its favorable placental transfer profile and minimal CYP450 metabolism interference. NSAIDs, however, inhibit prostaglandin synthesis, which compromises renal perfusion in the fetal unit-hence the FDA’s black box warning post-20 weeks. The emerging data on neurodevelopmental correlates with prolonged acetaminophen exposure warrants prospective cohort monitoring, particularly in the context of polypharmacy exposure. Always consider the therapeutic index and gestational pharmacokinetics before any intervention.
November 22, 2025 AT 03:01
Noah Fitzsimmons
Oh wow, so now we're treating pregnant women like fragile glass figurines that might shatter if they sneeze too hard? I mean, I get it, but let's not turn every cold into a biohazard emergency. My wife took Advil in week 8 and now my kid's a genius. Maybe the real danger is overmedicating with fear.
Also, why are we still using 'natural' like it's a medical credential? My grandma cured everything with whiskey and a hot iron. Who's to say that's worse?
November 22, 2025 AT 17:34
Clifford Temple
Look, I don't care what some study says. If you're American, you take what you need to function. This whole 'ask your doctor' thing is just government overreach wrapped in pink ribbons. You think your doctor gives a damn? They're too busy billing insurance to care if you took Tylenol or Tums. Just take the damn pill. If it's on the shelf, it's legal. If it's legal, it's fine. End of story.
Stop scaring women into paralysis. We're not lab rats. We're mothers.
November 24, 2025 AT 10:45
Corra Hathaway
YAS QUEEN. This is the kind of info we NEED. 🙌 I took Zyrtec for 3 months and felt like a human again. No more sneezing through my prenatal yoga. And yes, I read the label. No more 'Cold & Flu' for me - that stuff is a minefield. 🚫💊
Also, Tums are my bestie. I keep a bag in my purse like it's snacks. If you're not using saline spray for congestion, you're doing it wrong. So simple. So safe. So much better than feeling like a swamp monster.
Love this post. Save it. Print it. Tape it to your mirror. You got this, mama 💖
November 24, 2025 AT 14:34
Shawn Sakura
Thank you for this. I was so nervous about taking anything during my first trimester. I ended up just resting and drinking water and it worked. I didn't know that even some vitamins could interact. I thought my prenatal was enough. Turns out I was taking extra iron and it was giving me constipation worse than a toddler's tantrum. 😅
Also, I didn't realize that 'alcohol-free' cough syrup could still have alcohol. I'm so glad I checked. I'm keeping a log now. It's weird but kinda empowering. Like I'm in charge of my body, not the drug aisle.
November 25, 2025 AT 12:52
Paula Jane Butterfield
As a nurse who's worked in OB for 18 years, I can't tell you how many women come in terrified because they took one ibuprofen before they knew they were pregnant. Let me say this: one dose is not going to hurt your baby. Panic is the real enemy here.
What matters is what you do next. Write it down. Talk to your provider. Don't hide it. We've seen it all. We're not here to judge. We're here to help you make the next best choice.
Also - if you're using essential oils for 'natural relief,' please, please, please check with your provider first. Some of those are stronger than prescription meds. I've seen women hospitalized from lavender oil overdose. Yes, really.
You're not alone. We've got you.
November 26, 2025 AT 17:53
Simone Wood
Okay but let's be real - why is it that every time a woman gets pregnant, the entire world suddenly thinks she's incapable of making decisions? I'm a scientist. I read studies. I know what's in the bottle. I don't need a 12-page guide to tell me not to take Sudafed. I'm not a child. I'm a pregnant woman with a brain.
And yet here we are, being lectured like we're about to poison our babies by breathing too hard. It's exhausting. The real danger isn't the medication - it's the shame, the fear-mongering, the assumption that we're all just one wrong pill away from disaster.
Trust us. We're doing our best.
Also - who wrote this? It reads like a corporate wellness pamphlet. I need more honesty. Less marketing. Less 'you're not alone.' I'm not a marketing segment. I'm a person.
November 27, 2025 AT 17:36