When you can’t sleep, your mind doesn’t rest. It spins. Worrying. Ruminating. Replaying the same thoughts over and over. For people with depression or anxiety, this isn’t just a bad night-it’s a cycle that gets worse with every missed hour. Insomnia isn’t just a symptom of these conditions. It’s a driver. And treating it doesn’t just help you sleep better-it can change the course of your mental health.
Why Insomnia Isn’t Just a Side Effect
For years, doctors treated insomnia as a side effect of depression or anxiety. If you were sad or anxious, you probably couldn’t sleep. So they focused on the mood disorder first. But research now shows that’s backward. Insomnia doesn’t just happen because you’re depressed-it makes depression worse, and it can even trigger it. A 2025 study in Frontiers in Psychiatry found that people with chronic insomnia are 40 times more likely to develop severe depression than those who sleep well. That’s not correlation. That’s causation. When your brain doesn’t get enough rest, stress hormones like cortisol, ACTH, and CRH stay elevated. Your nervous system stays stuck in high gear. Your mood regulation systems break down. Over time, this rewires your brain to be more sensitive to negative thoughts and less able to recover from stress. The same is true for anxiety. Insomnia keeps your threat detection system on high alert. You start associating your bed with worry instead of rest. You lie there thinking, “What if I don’t sleep again?” That fear becomes a habit. And habits like that feed anxiety-making it harder to calm down, even when you’re not actively worried.The Gold Standard: CBT-I
The most effective, evidence-backed treatment for insomnia in people with depression or anxiety is CBT-I-Cognitive Behavioral Therapy for Insomnia. It’s not a pill. It’s a structured, time-limited therapy that targets the thoughts and behaviors keeping you awake. CBT-I typically lasts 6 to 8 weeks, with weekly 50- to 60-minute sessions. It’s not about counting sheep or drinking chamomile tea. It’s about retraining your brain and body to associate bed with sleep-not stress, not worry, not staring at the ceiling. Here’s how it works:- Stimulus control: You only go to bed when you’re sleepy. If you’re not asleep in 20 minutes, you get up and leave the bedroom. You come back only when sleepy again. This breaks the link between bed and frustration.
- Sleep restriction: You limit the time you spend in bed to match how much you’re actually sleeping. If you’re only sleeping 5 hours, you’re only allowed in bed for 5 hours. This builds sleep pressure so you fall asleep faster and stay asleep longer. It’s uncomfortable at first-65% of people report feeling more tired in the first week-but it works.
- Relaxation techniques: Diaphragmatic breathing, progressive muscle relaxation, and mindfulness practices help calm the nervous system before bed.
- Cognitive therapy: You identify and challenge beliefs like, “If I don’t sleep 8 hours, I’ll be useless tomorrow,” or “I’ll never be able to sleep again.” These thoughts keep anxiety high and make sleep impossible.
What the Science Says
A 2023 systematic review in Sleep journal analyzed 186 studies and found that people who completed CBT-I had significantly lower rates of developing major depressive disorder. Those who fully recovered from insomnia were 83% less likely to develop depression later. Even more telling: those who got CBT-I but didn’t fully recover their sleep still had a 41% lower risk than those who got no treatment. The same review found that CBT-I improved depression symptoms as much as antidepressants-without the side effects. In fact, a 2018 meta-analysis in Depression and Anxiety showed CBT-I had a larger effect on reducing depression than sleep education or placebo. The effect size? -1.29 on the Hamilton Depression Scale. That’s a big jump. And it lasts. Unlike sleeping pills, which wear off after a few weeks, CBT-I creates lasting change. A 2024 study in JAMA Psychiatry showed that people with depression and insomnia who got CBT-I plus sertraline had 40% higher remission rates than those who only took the medication. CBT-I didn’t just help them sleep-it helped them stay well.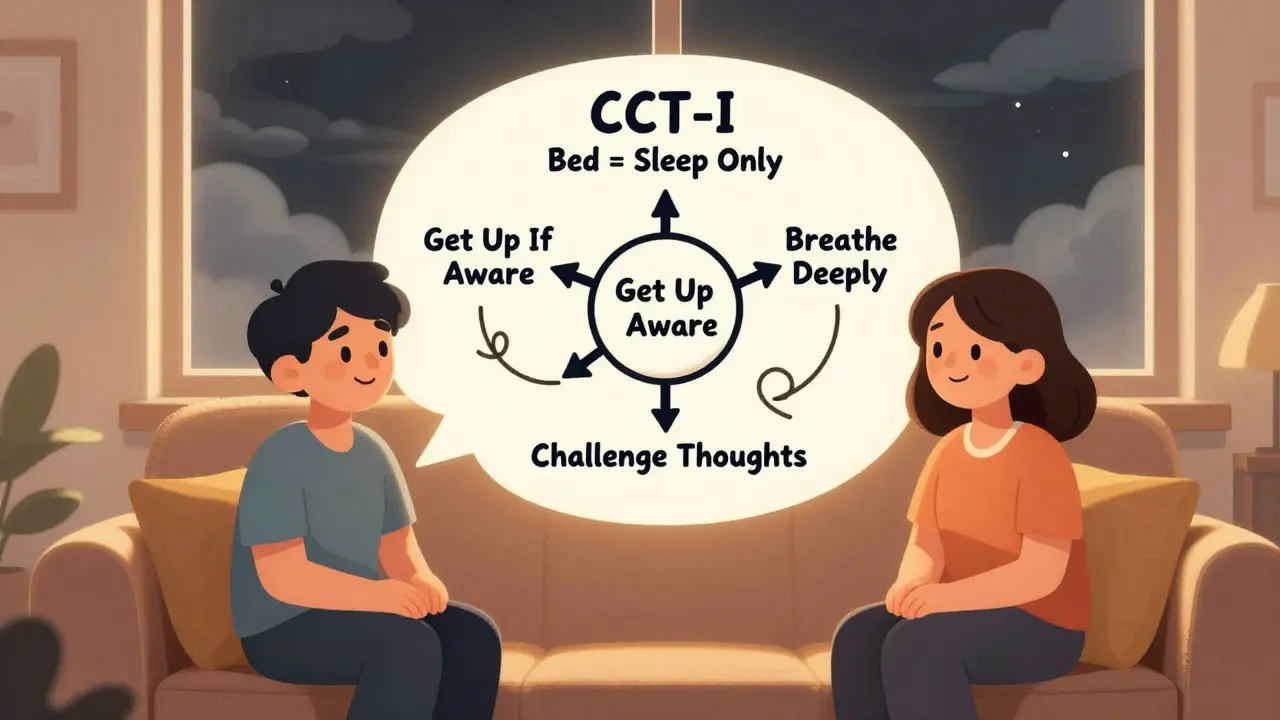
Digital CBT-I: Therapy You Can Access
Not everyone can see a therapist. There aren’t enough trained CBT-I providers-only about 1-2% of U.S. psychologists are certified. Insurance often doesn’t cover it. That’s where digital platforms come in. Programs like Sleepio and SHUTi deliver CBT-I through apps and websites. They use video lessons, interactive tools, and automated feedback to guide users through the same steps as in-person therapy. A study found that 76% of users saw clinically meaningful improvements in insomnia severity. One trial showed a 57% reduction in the odds of moderate-to-severe depression after using dCBT-I compared to just reading sleep tips. These platforms aren’t perfect. They don’t replace human support for people with severe depression or trauma. But for mild to moderate cases, they’re a game-changer. And they’re growing fast. Between 2019 and 2022, telehealth CBT-I use jumped 300%.Why Medications Fall Short
Pills like zolpidem (Ambien) or eszopiclone (Lunesta) help you fall asleep faster. But they don’t fix the underlying thoughts and habits keeping you awake. They also don’t prevent depression. A 2025 study in Nature Scientific Reports compared CBT-I and zolpidem. Both improved sleep and mood in the short term. But after six months, only the CBT-I group stayed better. The zolpidem group relapsed. Sleeping pills are a bandage. CBT-I is surgery. It removes the root cause.Who Benefits Most?
Not everyone responds the same way. About 30-40% of people don’t fully recover from insomnia after CBT-I. But that doesn’t mean it didn’t help. Even partial improvement reduces depression symptoms and lowers relapse risk. People who stick with it-those who complete sleep diaries, follow sleep schedules, and practice relaxation-see the best results. Adherence rates in clinical trials are 75-85%. And the more consistent you are, the better your mood improves. One study found a strong link between diary completion and depression improvement (r=0.42). It’s also worth noting: treating insomnia early can prevent depression from becoming chronic. That’s why Kaiser Permanente started screening all depression patients for insomnia in 2022. Those who got CBT-I saw a 22% drop in relapse rates.
The Bigger Picture
The global insomnia treatment market is expected to hit nearly $2 billion by 2030. But access is still a crisis. In the U.S., 30-35% of adults have insomnia symptoms. 10-15% meet the full diagnostic criteria. Yet fewer than 5% get CBT-I. The pandemic made it worse. In 2021, Columbia University found that one in three people had clinical insomnia-double pre-pandemic rates. And 68% of those people reported higher psychological distress. We’re treating the wrong thing. We’re giving antidepressants to people whose brains are exhausted from lack of sleep. We’re treating the fire, not the spark.What You Can Do Right Now
If you’re struggling with sleep and depression or anxiety:- Start a sleep diary. Write down when you go to bed, when you wake up, how long you were awake, and how you felt the next day.
- Get out of bed if you’re not asleep after 20 minutes. Go to another room, sit quietly, and come back only when sleepy.
- Limit caffeine after 2 p.m. Avoid alcohol before bed-it fragments sleep.
- Try a free digital CBT-I program like Sleepio (offered in some countries through public health systems) or SHUTi.
- Ask your doctor or therapist: “Can you refer me to a CBT-I provider?” If they don’t know what you’re talking about, ask for a referral to a sleep specialist.
It’s Not About Sleeping More. It’s About Sleeping Better.
You don’t need to sleep 8 hours to feel well. You need to sleep without fear. Without guilt. Without the dread of another sleepless night. Treating insomnia isn’t a luxury. It’s a core part of mental health recovery. And for people with depression or anxiety, it might be the most powerful tool they haven’t tried yet.Change doesn’t happen overnight. But if you’re willing to stick with it for six weeks, your brain might just learn how to rest again.


Jacob Milano
Man, this hit different. I used to lie there for hours, my brain like a broken record playing every embarrassing moment since middle school. Then I tried CBT-I through Sleepio-no magic pills, just dumb stuff like getting up when I couldn’t sleep. First week? I wanted to quit. Second week? I slept 4 hours. Third week? I actually woke up feeling human. Now I don’t even think about sleep anymore. Weird, right? That’s the point.
January 3, 2026 AT 07:02
Aaron Mercado
THIS IS THE MOST IMPORTANT THING YOU’LL READ THIS YEAR!!! Seriously, people are still taking Ambien like it’s candy??!!? CBT-I isn’t just ‘therapy’-it’s a full-system reboot for your brain!! You think depression is ‘chemical imbalance’? NO-it’s your nervous system screaming from sleep deprivation!!! And if your doctor doesn’t know CBT-I, FIRE THEM!!!
January 3, 2026 AT 10:08
saurabh singh
Bro, I’m from India, and here, people still think sleep problems = weak mind. My uncle told me ‘just drink warm milk and pray.’ I did CBT-I via app-no therapist, no stigma. Lost 30 pounds because I stopped eating at midnight from anxiety. Now I coach my cousins through it. Sleep isn’t luxury. It’s survival. And yes, it works. Try it. No excuses.
January 3, 2026 AT 13:36
Dee Humprey
For anyone scared to start CBT-I: it’s not about perfection. Missed a night? Didn’t do your diary? That’s fine. Just show up. I did this while working night shifts and grieving my mom. Some days I just wrote ‘I was tired’ in my log. That counted. Progress isn’t linear. It’s messy. And it’s still progress. 💙
January 4, 2026 AT 07:04
John Wilmerding
While the empirical evidence supporting CBT-I is robust and well-documented across multiple peer-reviewed journals, it is worth noting that accessibility remains a significant structural barrier. The current distribution of certified practitioners is disproportionately concentrated in urban centers, and socioeconomic disparities prevent equitable uptake. Furthermore, while digital platforms offer scalability, they may lack the nuanced therapeutic alliance necessary for individuals with comorbid trauma. A multi-tiered public health intervention is required.
January 5, 2026 AT 11:14
Peyton Feuer
Just wanted to say I tried the 20-minute rule and it felt weird at first-like I was abandoning my bed. But after a week, I stopped dreading it. Now I read in the living room or just sit with my eyes closed. No pressure. No guilt. I used to think sleep was something I had to force. Turns out, it’s something you let happen. Small shift. Huge difference.
January 6, 2026 AT 17:18
Siobhan Goggin
I wish this had been around when I was 22. I spent five years on antidepressants that made me feel like a zombie. Then I got diagnosed with insomnia and started CBT-I. My therapist said, ‘Your brain isn’t broken-it’s exhausted.’ I cried. That was the first time someone didn’t treat me like I was broken. I’m not cured, but I’m not drowning anymore.
January 8, 2026 AT 07:51
Vikram Sujay
The philosophical underpinning of this approach is profound. Modern medicine treats symptoms as entities to be suppressed, rather than signals to be understood. Insomnia is not a disorder of sleep, but a disorder of meaning-the mind’s refusal to surrender to rest because it has not been allowed to process its burdens. CBT-I, in its quiet discipline, restores agency. It does not heal the soul; it creates the space for the soul to heal itself.
January 9, 2026 AT 11:14
Jay Tejada
Yeah sure, CBT-I works… if you’re not broke, not working two jobs, and don’t have a kid who wakes up screaming at 3 a.m. I get it. It’s great for people who have time and privilege. Meanwhile, I’m drinking cold coffee at 2 a.m. while my toddler screams about a dream about a dragon. So yeah. Thanks for the advice. 🤷♂️
January 11, 2026 AT 07:29
Shanna Sung
CBT-I is a scam. Big Pharma doesn’t want you to know this, but sleep tech companies are secretly funded by the same people who make antidepressants. They want you to think you need ‘therapy’ so you’ll keep buying apps and subscriptions. Real solution? Turn off all screens, sleep in a bunker, and live off the grid. That’s what they don’t want you to know.
January 12, 2026 AT 11:47
Connor Hale
My favorite part? The part where they say you don’t need 8 hours. I spent years thinking I was failing because I only slept 5.5. Turns out, my brain just needed to stop panicking about the other 2.5. I still wake up once. But now I don’t panic. I just breathe. And that’s enough.
January 14, 2026 AT 10:20
Jacob Milano
@6564 - I hear you. I was working two jobs too. That’s why I started with just one thing: getting up after 20 minutes. No diary. No apps. Just… get up. It didn’t fix everything. But it broke the panic cycle. And that was the first real win. You don’t need to do it all. Just do one thing. Then another. That’s how you rebuild.
January 15, 2026 AT 22:24