When you’re on antibiotics and your stomach starts acting up, it’s tempting to grab an antacid. Tums, Maalox, Mylanta - they’re everywhere. But if you take them at the same time, you could be wasting your antibiotic. Not just a little - we’re talking up to 90% less effectiveness in some cases. This isn’t a myth. It’s a well-documented, clinically proven interaction that’s costing people their treatment success - and it’s entirely preventable.
Why Antacids Kill Antibiotic Absorption
Antacids work by neutralizing stomach acid. That’s good for heartburn. But your antibiotics? They need that acid to dissolve properly. Some, like doxycycline and ciprofloxacin, rely on a low pH to even begin being absorbed. When you swallow an antacid, you’re turning your stomach into a near-neutral environment. That alone cuts absorption.
But there’s something worse happening: chelation. Antacids containing aluminum, magnesium, or calcium don’t just change pH - they bind directly to certain antibiotics. Think of it like a magnet pulling iron filings away from your path. These metal ions latch onto tetracycline and fluoroquinolone antibiotics, forming a solid, insoluble compound that your body can’t absorb. It just passes through you, useless.
Studies show ciprofloxacin’s absorption drops by up to 90% when taken with antacids containing aluminum or magnesium. Doxycycline? Around 30-50% less. Even amoxicillin, which is less affected, still loses 15-20% of its potency. That’s not a small risk. If you’re treating a urinary tract infection or pneumonia, that drop could mean the difference between clearing the infection and needing a second round - or worse.
Which Antibiotics Are Most at Risk?
Not all antibiotics are equally vulnerable. Here’s who’s in danger:
- Fluoroquinolones - ciprofloxacin, levofloxacin, moxifloxacin. These are the worst offenders. They bind tightly to metals. Studies show up to 90% absorption loss. Separation time: 4 hours after or 2 hours before antacids.
- Tetracyclines - doxycycline, tetracycline, minocycline. These are also highly affected. Doxycycline, commonly used for acne and Lyme disease, sees 50-70% less absorption. Separation time: 2-3 hours.
- Some sulfonamides - like sulfamethoxazole. Less studied, but still show reduced absorption. Best to separate.
Now, the good news: some antibiotics barely care.
- Beta-lactams - amoxicillin, ampicillin, cephalexin. These are mostly unaffected. A 15-20% drop happens, but it rarely leads to treatment failure in healthy people. Still, separating by 1-2 hours is ideal.
- Macrolides - azithromycin, clarithromycin. Minimal interaction. Two hours separation is a safe precaution.
- Metronidazole - no meaningful interaction. You can take it with antacids without worry.
That’s why knowing your exact antibiotic matters. If you’re on ciprofloxacin for a UTI, timing isn’t optional - it’s life-saving. If you’re on amoxicillin for a sinus infection, you’ve got a little more flexibility - but why risk it?
The Timing Rules That Actually Work
"Just take them apart" isn’t enough. You need specifics.
The FDA, NHS, and Cleveland Clinic all agree on these windows:
- For fluoroquinolones (ciprofloxacin, levofloxacin): Wait 4 hours after taking an antacid, or take the antibiotic 2 hours before the antacid.
- For tetracyclines (doxycycline): Separate by 2-3 hours. Take the antibiotic on an empty stomach, at least 1 hour before food - and keep antacids out of that window.
- For amoxicillin, cephalexin: 1-2 hours separation is sufficient. Still, avoid taking them together.
- For azithromycin, metronidazole: No strict separation needed, but if you’re unsure, go with 2 hours.
Here’s a simple trick: if you take your antibiotic in the morning on an empty stomach, wait until after lunch to take your antacid. If you take your antibiotic at night, avoid antacids after dinner. Most people take antacids after meals - that’s your cue to schedule antibiotics before meals instead.
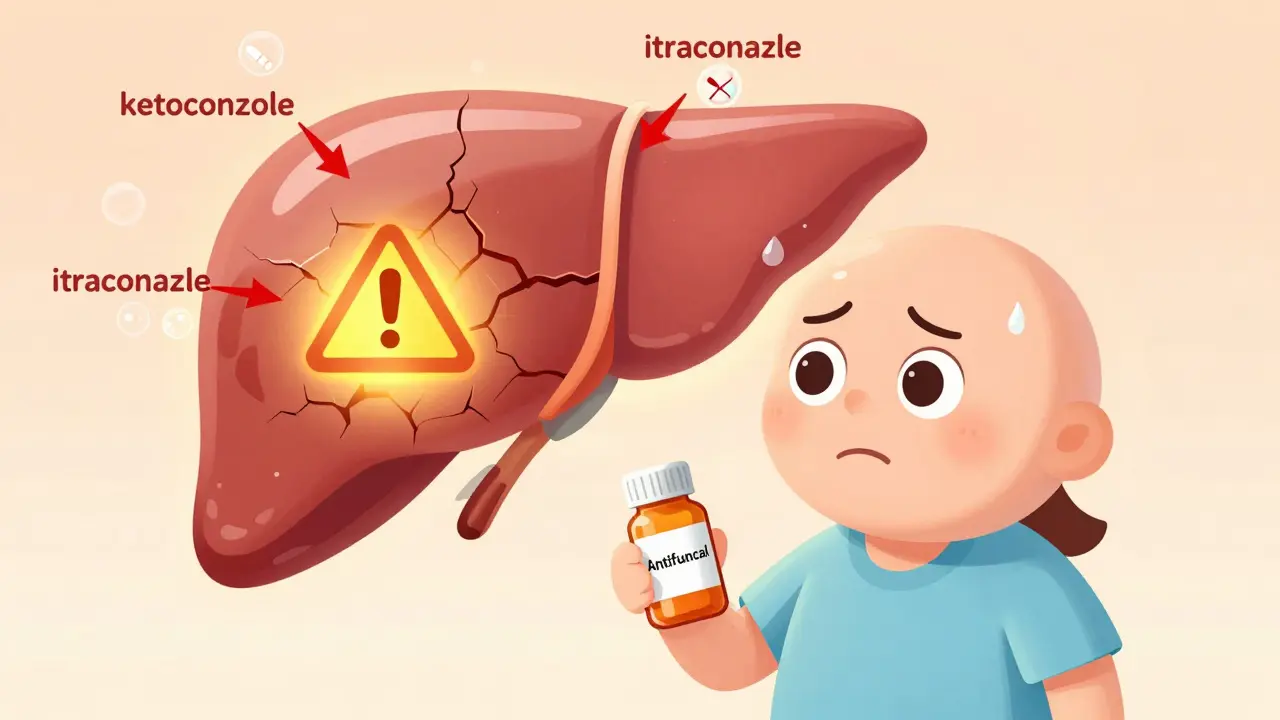
What About Proton Pump Inhibitors and H2 Blockers?
Many patients switch from antacids to daily acid reducers like omeprazole (Prilosec) or famotidine (Pepcid). Are they safer?
Yes - but not perfectly. PPIs and H2 blockers also raise stomach pH, so they can still interfere, though less dramatically. A 2023 study found that switching from antacids to omeprazole cut antibiotic treatment failure rates from 27% to just 9% in patients needing both drugs. That’s a huge win.
Still, even with PPIs, it’s best to separate them from high-risk antibiotics by 2 hours. They’re not as bad as Tums, but they’re not harmless either.
Real-World Consequences: What Happens When You Get It Wrong
It’s not theoretical. In 2021, the FDA reviewed data from 15,000 patients. Those who took ciprofloxacin with antacids within 2 hours had a 22% higher chance of treatment failure. That means recurring UTIs, longer sick days, and more doctor visits.
On Reddit, a physician shared: "I had five patients with recurring UTIs. All were taking ciprofloxacin with Tums. Once we spaced them out by 4 hours - boom. Infection cleared."
Dr. Sarah Thompson at Johns Hopkins calls this one of the top 10 preventable causes of antibiotic failure in outpatient care. That’s not a minor oversight. That’s a systemic gap.
And it’s expensive. In the U.S. alone, improper timing of these drugs leads to an estimated $1.2 billion in extra healthcare costs each year - from repeat prescriptions to hospitalizations for resistant infections.
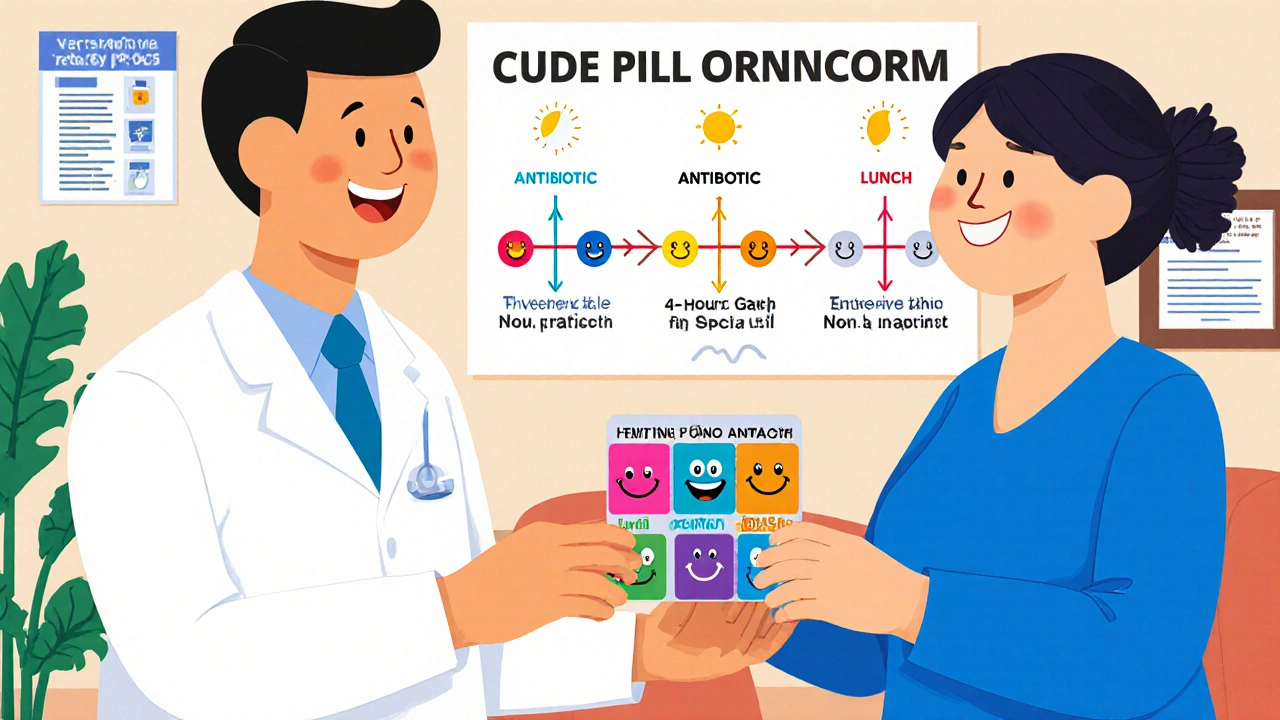
How to Actually Remember the Timing
People forget. Especially older adults on five or six meds a day. That’s why simple tricks work best.
- Use a pill organizer with time slots. Label each compartment: "AM Antibiotic," "Lunch," "PM Antibiotic," "Evening Antacid."
- Set phone alarms. Two alarms: one for antibiotic, one for antacid. Label them clearly: "Cipro - Take Now" and "Tums - Wait 4 Hours."
- Ask your pharmacist. Most will print out a simple timing chart. Many pharmacies now include this in their digital prescription notes.
- Use MyMedSchedule or Medisafe. These apps have built-in interaction alerts. If you input ciprofloxacin and Tums, they’ll flash a warning and suggest a schedule.
A Mayo Clinic study found that patients given a visual timeline - a simple diagram showing "Antibiotic → 4-hour gap → Antacid" - had 37% fewer timing errors. A picture beats a paragraph every time.
What’s New? Better Antibiotics Are Coming
In May 2023, the FDA approved a new version of ciprofloxacin called Cipro XR-24. It’s designed to absorb better even with antacids. In trials, it only lost 8% absorption - compared to 90% for the old version. That’s a game-changer.
Also, new guidelines from the American Society of Health-System Pharmacists now differentiate between antacid types. Calcium-based antacids (like Tums) require longer separation (4 hours) than magnesium-based ones (2 hours) for fluoroquinolones. This level of detail is finally making its way into clinical practice.
And researchers are looking ahead. A 2023 University of Pittsburgh study found that genetic differences in gastric emptying time affect how quickly drugs move through the stomach. In the future, your DNA might determine your ideal timing window.
Bottom Line: Don’t Guess. Separate.
If you’re on antibiotics, don’t assume antacids are harmless. Check the label. Ask your pharmacist. Know your drug class. If it’s ciprofloxacin or doxycycline, you need at least a 2-hour gap - and 4 hours is safer. If it’s amoxicillin, 1-2 hours is fine.
Antibiotics don’t work if they don’t get absorbed. Antacids aren’t the enemy - but timing is everything. Get it right, and you treat the infection. Get it wrong, and you’re just feeding resistance.
One extra dose, one missed gap - and you might be back in the doctor’s office. Don’t let a simple mistake undo your treatment.
Can I take Tums with amoxicillin?
Yes, but not at the same time. Amoxicillin is less affected by antacids than other antibiotics, but taking them together can still reduce absorption by 15-20%. To be safe, wait at least 1-2 hours after taking amoxicillin before taking Tums or any antacid. If you’re taking amoxicillin twice a day, take it on an empty stomach in the morning and evening, and use antacids only after lunch or dinner.
How long should I wait after taking ciprofloxacin before taking an antacid?
Wait at least 4 hours after taking ciprofloxacin before taking an antacid containing aluminum, magnesium, or calcium. If you need to take the antacid first, wait at least 2 hours before taking your ciprofloxacin. This 4-hour window is critical - ciprofloxacin absorption drops by up to 90% if taken too close to antacids. Don’t rely on feeling better - even if symptoms improve, the antibiotic may not have reached effective levels in your body.
Does omeprazole (Prilosec) interact with antibiotics the same way as antacids?
Omeprazole raises stomach pH like antacids, so it can reduce absorption of some antibiotics - especially tetracyclines and fluoroquinolones. But the effect is usually milder. Still, it’s safest to separate omeprazole from high-risk antibiotics by at least 2 hours. For patients needing long-term acid suppression while on antibiotics, switching from daily antacids to omeprazole can actually reduce treatment failure rates by more than half, according to a 2023 study.
Can I take antacids with azithromycin or metronidazole?
Azithromycin has minimal interaction with antacids, but a 2-hour separation is still recommended as a precaution. Metronidazole, on the other hand, shows no significant interaction. You can take metronidazole with antacids without worrying about reduced effectiveness. Always check your specific antibiotic’s label - but if you’re on metronidazole for a bacterial infection or parasitic condition, you’re safe to use antacids as needed.
What if I accidentally took my antibiotic with an antacid?
Don’t panic, but don’t ignore it either. If you took them together once, it’s unlikely to cause immediate harm - but it may reduce the antibiotic’s effectiveness. Skip your next antacid dose until you’ve waited the full separation time. If you’re on a short course (5-7 days), continue the antibiotic as prescribed. If symptoms don’t improve or get worse, contact your doctor. You may need a repeat course or a different antibiotic. For high-risk drugs like ciprofloxacin, one mistake can be enough to trigger treatment failure.



kora ortiz
Stop mixing meds like cocktail ingredients. If you're on cipro, wait 4 hours before Tums. Simple. No excuses. Your body isn't a lab experiment.
November 18, 2025 AT 14:55
Kathryn Ware
I literally just had my third UTI in 8 months because I didn’t know this 😭 I was taking cipro at night and Tums after dinner like a normal person… turns out I was just feeding the bacteria 🤦♀️ I started spacing them out 4 hours apart and holy cow, no recurrence in 3 months now. Also, I use Medisafe app and it sends me little bell notifications like ‘CIPRO TIME 🚨’ and ‘TUMS IN 4 HRS 🍬’ - game changer. If you’re on antibiotics, get that app. Your future self will thank you with a clean bladder and zero repeat prescriptions. 💪❤️
November 19, 2025 AT 21:57
Kyle Swatt
It’s funny how we treat our bodies like machines that run on pills and ignore the fact that stomach acid isn’t just ‘burny stuff’ - it’s the first gatekeeper of digestion. We’ve been conditioned to fear acid, to crush it with chalky tablets like it’s the enemy. But the truth? Acid is the silent warrior keeping pathogens out and meds in. When you neutralize it, you’re not just helping your heartburn - you’re handing your infection a free pass. We’re not just medicating. We’re meditating on the paradox of modern medicine: we fix one thing and break another because we don’t understand the ecosystem we’re tampering with. 🤔
November 20, 2025 AT 03:16
Kiran Mandavkar
Wow. Another ‘medical advice’ post from someone who clearly never read a pharmacology textbook. ‘90% less absorption’? Where’s your citation? That’s not a study - that’s a blog post masquerading as science. You’re scaring people with cherry-picked numbers while ignoring bioavailability studies from JAMA and The Lancet. If you’re going to post this, at least cite the actual trials. Otherwise, you’re just adding noise to the noise.
November 20, 2025 AT 07:33
Shannon Hale
OH MY GOD. I just realized I’ve been taking doxycycline with Tums for TWO YEARS. I thought it was fine because I ‘felt fine.’ But my acne never cleared. My Lyme symptoms kept coming back. I was literally poisoning my own treatment. I’m so mad I cried. Now I’ve got a pill organizer with color-coded slots and alarms named ‘ANTIBIOTIC MODE ACTIVATED’ and ‘TUMS IS A TRAITOR.’ I’m never doing this again. If you’re reading this and you’re on antibiotics - STOP. LOOK. WAIT. Your life is not worth a 20-minute delay.
November 22, 2025 AT 03:08
saurabh lamba
why do we even take antibiotics anymore? if your body can't handle a little acid, maybe you're just weak. also tums are just calcium carbonate - it's like eating chalk. who even uses this stuff? 🤷♂️
November 23, 2025 AT 16:38
Deb McLachlin
Thank you for this comprehensive and clinically grounded overview. The differentiation between fluoroquinolones, tetracyclines, and beta-lactams is particularly valuable. I would add that the 2023 ASHP guidelines referenced here are now included in the 2024 Lexicomp drug interaction module, which many hospital pharmacies have integrated into their electronic prescribing systems. Pharmacists are increasingly being trained to flag these interactions at the point of dispensing - a significant improvement in patient safety. For those on polypharmacy regimens, consulting a clinical pharmacist is not just advisable - it is a standard of care.
November 24, 2025 AT 09:37
Holli Yancey
I’ve been on azithromycin for a week now and I took a Tums last night because my stomach was upset. I didn’t think it mattered since I read somewhere it’s ‘low risk’… but now I’m second-guessing everything. I don’t want to mess up my treatment. I just want to feel better without feeling guilty. Is it too late? Should I skip my next dose? I’m just so tired of having to be a pharmacist for myself.
November 26, 2025 AT 03:23
Tarryne Rolle
Isn’t it ironic that we’ve created a system where the very tools meant to heal us - pills, pills, and more pills - require a PhD in pharmacokinetics just to use correctly? We’ve outsourced our bodies to Big Pharma, then blamed ourselves when things go wrong. The real problem isn’t the antacid. It’s the belief that health can be reduced to a schedule. What if your body doesn’t want to be timed? What if the real solution isn’t spacing out drugs, but healing the gut that needs them in the first place? We treat symptoms like enemies, not signals. And that’s why we keep losing.
November 27, 2025 AT 11:19
Gordon Mcdonough
AMERICA IS BECOMING A COUNTRY OF OVERMEDICATED COWARDS WHO CAN’T HANDLE A LITTLE HEARTBURN WITHOUT CHEWING A WHITE TABLET LIKE A COW EATING STONE. YOU WANT TO BE HEALTHY? EAT LESS SPICY FOOD. STOP TAKING ANTIBIOTICS FOR A COUGH. YOU THINK YOUR BODY CAN’T HANDLE ACID? THEN YOU’RE THE PROBLEM. THIS POST IS JUST ANOTHER WAY PHARMA MAKES MONEY OFF YOUR FEAR. TUMS ARE CHEAP. ANTIBIOTICS ARE EXPENSIVE. WHO BENEFITS? NOT YOU.
November 27, 2025 AT 15:50
Eric Healy
Wait so if I take cipro at 8am I can have tums at 12pm? what if i take it at night? do i wait till 4am? i dont wanna wake up to take tums
November 28, 2025 AT 02:55
Kathryn Ware
@4102 - YES you wait till 12pm if you took it at 8am. If you take cipro at night, don’t take Tums after dinner - take the cipro before dinner, then wait 4 hours. So eat dinner at 6pm, take cipro at 7pm, and don’t touch Tums until 11pm. Or better yet - take your cipro in the morning on an empty stomach, then have your Tums with lunch. It’s easier than you think. I used to think I’d have to wake up at 4am too… then I just changed my routine. Now I take my antibiotic with my coffee, and my Tums with my avocado toast. No alarms needed. 🥑☕
November 28, 2025 AT 15:00