Imagine needing to spend two to three hours every day just to breathe. For decades, that was the reality for people with cystic fibrosis (CF). Thick, sticky mucus clogged their lungs, trapped bacteria, and led to constant infections. Their pancreas couldn’t digest food properly. Many didn’t live past childhood. But today, that story is changing - fast.
What Exactly Is Cystic Fibrosis?
Cystic fibrosis is a genetic disorder caused by mutations in the CFTR gene, a gene on chromosome 7 that controls how salt and water move in and out of cells. When this gene doesn’t work right, the body makes mucus so thick it clogs airways, ducts, and passageways. It’s not contagious. You can’t catch it. You’re born with it - and you need two faulty copies of the gene, one from each parent, to have the disease.People with just one copy are carriers. They don’t have symptoms but can pass the gene to their kids. About 1 in 25 people of Northern European descent carry a CF mutation. It’s less common in other groups, but it shows up everywhere. The most common mutation, called F508del, accounts for about 70% of all CF cases worldwide. But there are over 2,000 known mutations, and each can affect the body differently.
The symptoms aren’t just about breathing. CF hits multiple organs. In the lungs, mucus builds up, leading to chronic infections with bugs like Pseudomonas aeruginosa and Staphylococcus aureus. Over time, this causes scarring, bronchiectasis, and lung failure - the number one reason people with CF die. In the pancreas, mucus blocks enzyme ducts. About 85% of people with CF can’t digest food properly without taking enzyme pills with every meal. The liver can get damaged from bile duct blockages. And nearly all men with CF are infertile because they’re born without the tube that carries sperm.
The classic diagnostic test? A sweat test. If your sweat has more than 60 mmol/L of chloride, it’s a strong sign of CF. Most kids are now caught early thanks to newborn screening, which is standard in the U.S. and many other countries.
How CF Is Different From Other Lung Diseases
It’s easy to confuse CF with other respiratory conditions like Primary Ciliary Dyskinesia (PCD), a rare disorder where the tiny hair-like structures in the airways don’t move properly. Both cause chronic cough and infections. But the root causes are totally different.PCD is about broken cilia - the cleanup crew in your lungs. CF is about broken salt channels. In CF, the mucus is thick because it’s dehydrated. In PCD, the mucus is normal, but it doesn’t get cleared. That’s why treatments for PCD focus on physical clearance techniques, while CF now has drugs that fix the root problem.
CF is also unique because it’s one of the few genetic diseases where we’ve developed drugs that actually fix the faulty protein. That’s not true for most inherited lung conditions. That’s why CF has become a model for precision medicine - and why it’s now the most advanced area of treatment in respiratory genetics.
The Revolution: CFTR Modulator Therapies
Before 2012, treatment for CF was all about managing symptoms. Inhalers, antibiotics, chest physiotherapy, enzyme pills - it was a daily grind. Life expectancy? Around 30 years. Many kids didn’t make it to adulthood.Then came CFTR modulators, a new class of drugs that target the defective CFTR protein directly. These aren’t just pills - they’re molecular fixes. They help the protein fold right, open the chloride channel, or get to the cell surface where it’s needed.
The first one, ivacaftor (Kalydeco), was approved in 2012 for people with the G551D mutation. In trials, it boosted lung function by over 10%. That was huge. But it only helped about 4% of the CF population.
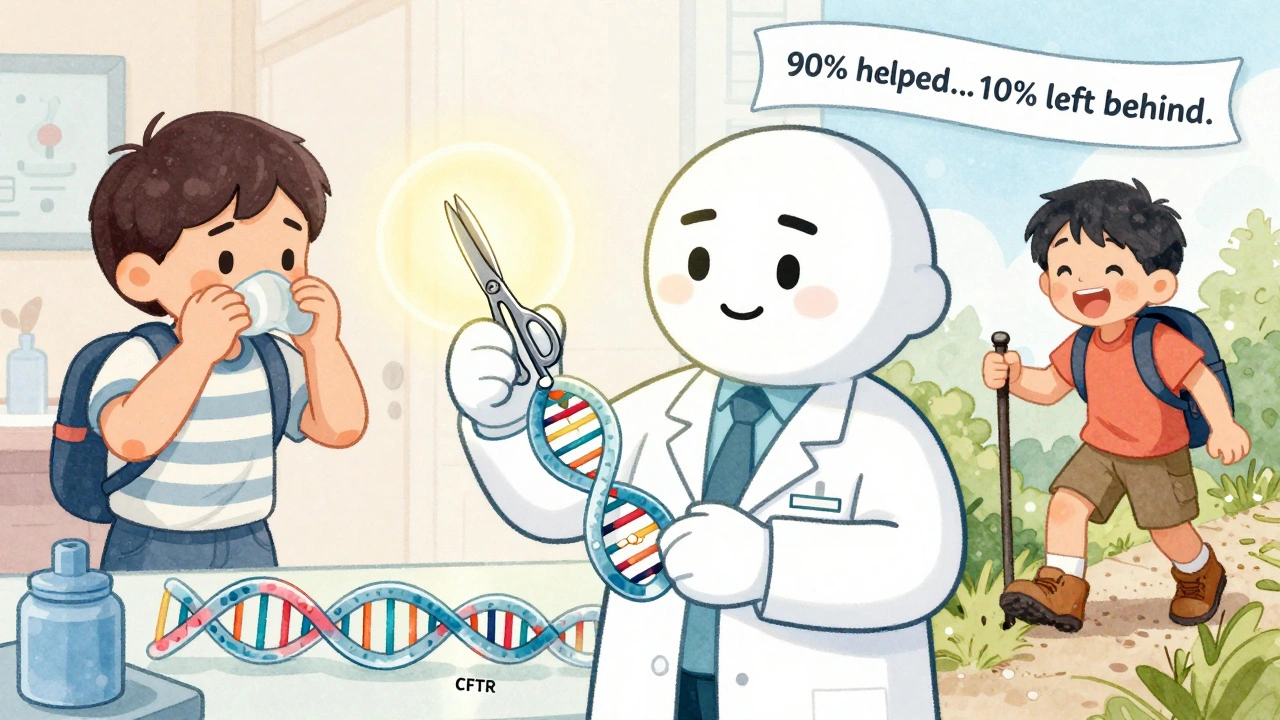
The real game-changer came in 2019 with Trikafta (elexacaftor/tezacaftor/ivacaftor). This triple combo works for people with at least one F508del mutation - which is about 90% of all CF patients. In clinical trials, it improved lung function by 13.8% and cut lung flare-ups by 63%. One patient in Australia told me their daily airway clearance went from 90 minutes to 20 minutes. They started gaining weight. They went back to work. They traveled. They felt like they had their life back.
Today, six CFTR modulators are approved. The Cystic Fibrosis Foundation says 90% of people in the U.S. now have access to at least one. Life expectancy has jumped to nearly 51 years. That’s a 37-year increase since the 1960s.

The Dark Side of Progress
But it’s not all sunshine. These drugs cost around $300,000 a year in the U.S. Even with insurance, many families pay $1,200 a month out of pocket. In low- and middle-income countries, less than 10% of people with CF can get these drugs. That means the gap between rich and poor with CF is wider than ever.And not everyone benefits. About 10% of people have mutations that don’t respond to current modulators. That’s tens of thousands of people still stuck with the old, grueling routines. Some report serious side effects - liver damage, cataracts, headaches. One study found 3.2% of users had to stop treatment because of liver enzyme spikes.
Then there’s the access gap. In the U.S., 85% of eligible patients get modulators. In Europe, it’s 45%. In many parts of Africa, Asia, and Latin America, it’s under 5%. The World Health Organization calls this a global health injustice. People with CF in wealthier countries are living into their 50s. In others, many still die in their teens.
What Daily Life Looks Like Today
Even with modulators, CF isn’t cured. Most people still need daily treatments. Airway clearance. Inhaled antibiotics. Pancreatic enzymes. Vitamins. Nutritional shakes. It’s still a full-time job.But it’s changed. People who used to be homebound are now hiking, going to college, having kids. One 28-year-old in Toronto told me she’s planning her wedding. She never thought she’d make it to 30. Now she’s thinking about retirement.
For those without modulators, the routine hasn’t changed. They still do chest physiotherapy with a vest or handheld device. They take 6-12 enzyme capsules with every meal. They’re on antibiotics every few months. They miss work. They get hospitalized. They live with the fear of their next lung infection.
What’s Next? The Pipeline of Hope
Scientists aren’t stopping. The Cystic Fibrosis Foundation is funding 15 new clinical trials. One is testing mRNA therapy for nonsense mutations - a type of mutation that stops protein production entirely. Another is using CRISPR gene editing to fix the CFTR gene at the DNA level. A third is developing new inhaled antibiotics to beat stubborn Pseudomonas infections.Trikafta was just approved for kids as young as 2. That means more children will grow up with better lung health from the start. And Vertex Pharmaceuticals, the company behind most modulators, is working on next-gen versions that might work for all mutations.
The Foundation has pledged $100 million to find treatments for the 10% left behind. That’s not charity - it’s science. Because if we can fix CF for 90%, why not the rest?
Support and Resources
You don’t have to face this alone. The Cystic Fibrosis Foundation runs 260 accredited care centers in the U.S. and offers 24/7 clinical advice. Online communities like CF Buddy Connect have over 12,500 active members. The annual International CF Conference brings together doctors, researchers, and families from 94 countries.For families, the biggest help is often practical: knowing how to do airway clearance right, which enzymes to use, when to call the doctor. Most care centers offer training sessions. And with modulators, adherence matters more than ever. Missing doses can mean losing the benefits.
Financial help is available too. Foundations offer copay assistance. Some countries have government programs. In Australia, the Pharmaceutical Benefits Scheme covers Trikafta - so cost isn’t the barrier it is in the U.S.
Final Thoughts
Cystic fibrosis used to be a death sentence. Now, it’s a chronic condition - one with a future. The science behind CFTR modulators is one of the greatest medical breakthroughs of the 21st century. It’s proof that targeting the root cause of a genetic disease can change everything.But progress isn’t fair. It’s uneven. The people who benefit most are those with money, access, and good healthcare systems. That’s the real challenge now: making sure the next generation of therapies doesn’t leave anyone behind.
Is cystic fibrosis curable?
No, cystic fibrosis is not yet curable. But CFTR modulator therapies can now control the disease so effectively that many people live nearly normal lifespans. Research into gene editing and mRNA therapies is ongoing, and a true cure may be possible in the coming decades.
Can you get cystic fibrosis if only one parent is a carrier?
No. CF is an autosomal recessive disorder, meaning you need two faulty copies of the CFTR gene - one from each parent. If only one parent is a carrier, the child might be a carrier too, but they won’t have the disease.
How do CFTR modulators work?
CFTR modulators fix the defective CFTR protein in different ways. Some help it fold correctly (correctors like tezacaftor), others help it open to let chloride through (potentiators like ivacaftor), and some do both. Trikafta combines three drugs to help the protein reach the cell surface and function properly.
Are CFTR modulators safe for children?
Yes. Trikafta is approved for children as young as 2 years old. Studies show it improves lung function and reduces infections in kids, with side effects similar to adults - mostly mild headaches, stomach upset, or liver enzyme changes. Regular monitoring is required.
Why are CFTR modulators so expensive?
They’re expensive because they’re developed for a small patient group (orphan drugs), require years of research, and are patented by a single company - Vertex Pharmaceuticals. The Cystic Fibrosis Foundation helped fund early research, but the drug’s pricing reflects market dynamics, not production cost. Many countries negotiate lower prices, but in the U.S., out-of-pocket costs remain high.
What happens if someone stops taking CFTR modulators?
If someone stops, their lung function typically declines within weeks to months. Symptoms like coughing, mucus buildup, and infections return. Weight loss and fatigue often follow. These drugs don’t cure CF - they manage it. Stopping means going back to the old, more aggressive treatment routine.
If you or someone you know has CF, the key is staying connected - to care teams, support groups, and the latest research. The future isn’t just about living longer. It’s about living better - and that future is already here for many.


Fern Marder
I just cried reading this. My cousin has CF and started Trikafta last year. She went from barely walking to hiking Mount Rainier. 🥹💪
December 3, 2025 AT 17:09
Carolyn Woodard
The mechanistic elegance of CFTR modulators is profound. The pharmacochaperoning effect of correctors like elexacaftor, coupled with potentiator kinetics of ivacaftor, represents a paradigm shift in allele-specific protein rescue. Yet the epistatic variability across >2000 mutations remains a formidable translational challenge.
December 4, 2025 AT 23:17
Allan maniero
I’ve got a mate in Manchester whose kid’s on Trikafta. He said the biggest change wasn’t the lung numbers-it was the silence. No more coughing fits at 3am. No more hospital bags packed by the door. Just… normal bedtime. That’s the real win, isn’t it?
December 5, 2025 AT 19:57
Anthony Breakspear
Man, these drugs are straight-up magic. I used to think CF was a life sentence. Now I see 25-year-olds planning weddings, hiking trails, and getting grad degrees. But let’s not sugarcoat it-$300k a year is a joke. If we can drop a billion on space telescopes, we can make this affordable. This ain’t just medicine, it’s justice.
December 5, 2025 AT 21:23
Zoe Bray
The clinical data supporting CFTR modulator efficacy is robust and statistically significant. However, the socioeconomic disparities in access, particularly across global healthcare systems, represent a critical ethical imperative requiring immediate policy intervention. The World Health Organization’s framing of this as a health injustice is not hyperbolic-it is empirically accurate.
December 6, 2025 AT 07:57
Girish Padia
Why should rich people get to live longer just because they live in America? We have kids dying in India because they can’t afford pills. This isn’t science-it’s capitalism with a stethoscope.
December 7, 2025 AT 07:42
Sandi Allen
Trikafta was funded by the Cystic Fibrosis Foundation… but who owns the Foundation? Who owns Vertex? Who owns the patents? It’s all connected. The same people who pushed for newborn screening now profit from lifelong dependency. You think this is progress? It’s a trap. They want you hooked. And they know it.
December 7, 2025 AT 18:16
Doug Hawk
i read somewhere that the 10 who dont respond to modulators mostly have nonsense mutations and that mrna therapy could fix that but like… has anyone tried just using crispr on embryos? like why are we treating symptoms when we could just fix the dna before birth? i know its edgy but like… why not
December 9, 2025 AT 12:13
John Morrow
Let’s be honest-the real breakthrough here isn’t the science. It’s the marketing. Vertex turned a rare disease into a billion-dollar product line. The 90% coverage stat? That’s cherry-picked from the U.S. and Western Europe. In the rest of the world? It’s a fantasy. The science is impressive. The capitalism? Not so much.
December 11, 2025 AT 00:00
Kristen Yates
I work with refugee families. One mother asked me if her son could get the pills. I had to tell her no. She didn’t cry. She just nodded. That silence hurt more than any scream.
December 11, 2025 AT 18:36
Saurabh Tiwari
in india we have no access but i know someone who got trikafta through a clinical trial in bangalore. he said the first week he felt like he could breathe for the first time since he was 5. i wish everyone could feel that
December 12, 2025 AT 05:26
Michael Campbell
America spends billions on this while our veterans can’t get basic care. This isn’t medicine. It’s a weapon. They’re selling hope to the rich and selling death to the rest. And we’re supposed to be grateful?
December 13, 2025 AT 07:37