Heart failure isn’t a single disease-it’s a condition that slowly steals your ability to breathe, move, and live normally. But here’s the good news: modern medicine has tools that don’t just manage symptoms-they save lives. Four drug classes form the backbone of treatment for heart failure with reduced ejection fraction (HFrEF): ACE inhibitors, ARNI, beta blockers, and diuretics. Together, they’ve cut death rates by up to 20% and hospital visits by over 20%. Yet, most people don’t get all four, even when they should.
What ACE Inhibitors Do-and Why They Still Matter
ACE inhibitors were the first real breakthrough in heart failure treatment. When they hit the market in the 1980s, doctors saw something shocking: patients weren’t just feeling better-they were living longer. The CONSENSUS trial in 1987 showed enalapril cut death risk by 27% in severe heart failure. That was revolutionary.
How do they work? They block the enzyme that turns angiotensin I into angiotensin II, a hormone that tightens blood vessels and makes the heart work harder. By stopping this, ACE inhibitors lower blood pressure, reduce strain on the heart, and slow damage. Common ones include enalapril, lisinopril, and ramipril.
But they’re not perfect. About 1 in 5 people get a dry, annoying cough-so persistent it makes them quit. Some develop high potassium levels, which can be dangerous. A rare but serious side effect is angioedema-swelling in the face or throat. If you’ve ever had this reaction to an ACE inhibitor, you can’t use ARNI either.
ARNI: The New Gold Standard Replacing ACEIs
If ACE inhibitors were the first big step, ARNI is the leap forward. Sacubitril/valsartan (brand name Entresto) was approved in 2015 after the PARADIGM-HF trial showed it beat enalapril. Patients on ARNI had 20% fewer deaths and 21% fewer hospital stays. That’s not a small gain-it’s the biggest improvement in heart failure meds in decades.
What makes ARNI different? It’s a combo drug. Valsartan blocks angiotensin like an ARB, but sacubitril blocks neprilysin, an enzyme that breaks down natural heart-protective hormones called natriuretic peptides. More of these peptides mean better fluid control, lower blood pressure, and less heart scarring.
It’s not for everyone. You must stop ACE inhibitors at least 36 hours before starting ARNI-otherwise, angioedema risk spikes. It’s also expensive: around $550 a month without insurance. But for most patients with HFrEF and an ejection fraction below 40%, it’s now the first choice over ACEIs. The 2022 AHA/ACC/HFSA guidelines say so clearly.
Beta Blockers: Slowing Down to Save the Heart
It sounds backwards-how can slowing your heart help a failing heart? But beta blockers aren’t just for high blood pressure. In heart failure, they protect the heart muscle from being overworked by stress hormones like adrenaline.
Three are proven: carvedilol, metoprolol succinate, and bisoprolol. The MERIT-HF and CIBIS-II trials showed each cut death risk by 30-35%. Carvedilol even improved ejection fraction in some patients-from 25% to 45% over 18 months, according to patient reports.
But they’re tricky to start. You begin at a tiny dose-like 3.125 mg of carvedilol twice a day-and wait weeks before increasing. If you jump too fast, you can make heart failure worse. Side effects include low blood pressure, slow heart rate, and fatigue. Many patients quit because they feel drained. But those who stick with it often say their energy returns after a few months. One Reddit user wrote: “I thought I’d never walk to the mailbox again. After six months on carvedilol, I hiked a trail with my grandkids.”
Diuretics: The Symptom Fixers
Diuretics don’t extend life. But they make life bearable. If you’re swollen, short of breath, or waking up at night needing to pee, diuretics are your relief.
Loop diuretics like furosemide, torsemide, and bumetanide are the go-to. They pull excess fluid out through your kidneys. Torsemide may be better than furosemide-studies show it leads to fewer hospital readmissions. Thiazides like hydrochlorothiazide are used for milder cases or combined with loops for stronger effect.
But there’s a catch. They can drain too much potassium and magnesium, leading to cramps, dizziness, or even dangerous heart rhythms. Many patients start taking supplements. One patient on PatientsLikeMe said: “Furosemide wiped me out until I added magnesium. Now I can walk without stopping.”
Spironolactone is a special case. It’s a diuretic, but also a mineralocorticoid receptor antagonist (MRA). It blocks aldosterone, a hormone that causes fluid retention and heart scarring. The RALES trial showed it cut death risk by 30%. But it can spike potassium levels-so you need regular blood tests.
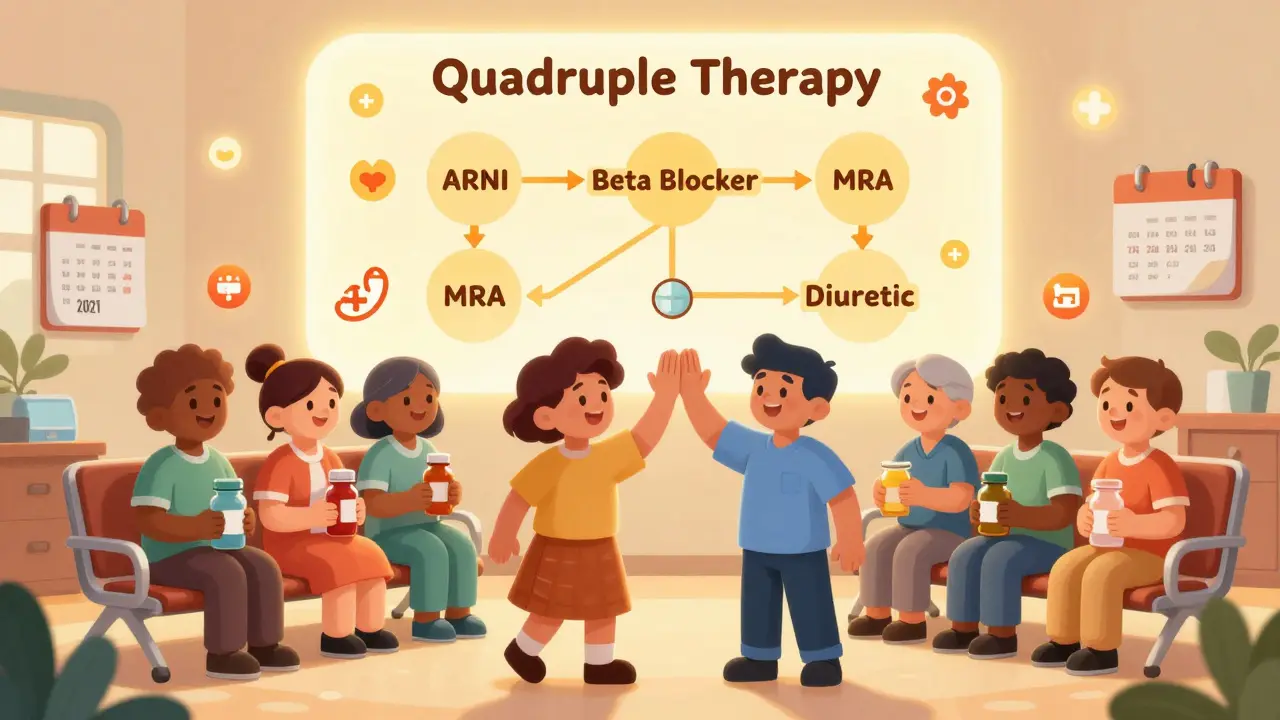
The Quadruple Therapy That Saves Lives
The best outcomes don’t come from one drug. They come from all four working together: ARNI (or ACEI/ARB), beta blocker, MRA, and SGLT2 inhibitor-with diuretics added as needed. This is called guideline-directed medical therapy (GDMT).
Yet, only 35% of eligible patients get all four within a year of diagnosis. Why? Cost, fear of side effects, lack of follow-up, and doctors not pushing hard enough. A 2021 study found that heart failure clinics with specialist teams achieved 85% adherence. General practices? Just 52%.
Even if you’re on ARNI and a beta blocker, skipping the MRA or SGLT2 inhibitor means you’re missing out on half the benefit. SGLT2 inhibitors like dapagliflozin and empagliflozin, originally for diabetes, now have strong evidence for all types of heart failure-even when the heart’s pumping normally.
What to Watch For and When to Call Your Doctor
Starting these meds is a marathon, not a sprint. You’ll need blood tests every 1-2 weeks after starting or changing doses. Watch for:
- High potassium (over 5.0 mmol/L)
- Worsening kidney function (creatinine up more than 30%)
- Low blood pressure (below 90 systolic)
- Severe dizziness or fainting
- Swelling in the face, lips, or tongue (call 911-this is angioedema)
Don’t stop meds because of side effects unless your doctor tells you to. Fatigue from beta blockers often fades. Cough from ACEIs can be swapped for ARNI. Low potassium from diuretics can be fixed with diet or supplements.
Real Patients, Real Results
Online forums like Reddit and PatientsLikeMe are full of stories that statistics can’t capture. One user switched from lisinopril to Entresto and said: “Within two weeks, I wasn’t gasping for air climbing stairs anymore.” Another said: “I hated the 5 a.m. bathroom trips from furosemide-until I switched to torsemide. Now I only go once at night.”
But cost is a real barrier. A 72-year-old in rural Texas told his doctor: “I can afford my insulin, but not my heart pills.” That’s why insurance prior authorization and patient assistance programs matter. Medicare covers 85% of ARNI-but you still need paperwork.
And here’s the kicker: the benefits don’t fade. The longer you stay on these drugs, the more your heart heals. Some patients see their ejection fraction climb from 20% to 50%-enough to get off the transplant list.
What’s Next for Heart Failure Treatment?
Research is moving fast. ARNI is now being tested in patients with mildly reduced heart function (HFmrEF)-and early data looks promising. Vericiguat, a new drug that helps the heart respond better to stress signals, is already approved as an add-on for worsening heart failure.
By 2027, experts predict ARNI will be first-line for 70% of HFrEF patients. But until then, the biggest gap isn’t science-it’s access. If you’re not on all four meds, ask why. If your doctor says you’re not a candidate, get a second opinion. You deserve the best chance to live longer, breathe easier, and enjoy your days.
Can I take ACE inhibitors and ARNI together?
No. You must stop ACE inhibitors for at least 36 hours before starting ARNI. Taking them together increases the risk of angioedema-a dangerous swelling of the face, lips, or throat. This is a strict safety rule backed by clinical trials and the 2022 AHA/ACC/HFSA guidelines.
Why do beta blockers make me so tired?
Beta blockers reduce your heart rate and blood pressure, which can lower energy levels, especially at first. Fatigue is common in the first 4-8 weeks. But many patients say their energy improves after that as their heart becomes stronger. Never stop them abruptly-talk to your doctor about adjusting the dose slowly.
Are diuretics dangerous long-term?
They’re safe if monitored. The main risks are low potassium, low sodium, and dehydration. Regular blood tests and staying hydrated help. Many patients take potassium or magnesium supplements. Torsemide is often preferred over furosemide because it’s more predictable and linked to fewer hospital readmissions.
Is ARNI worth the cost?
For most patients with HFrEF, yes. ARNI reduces hospital stays and death risk more than ACE inhibitors. While it costs about $550 a month without insurance, many programs help cover it. Medicare and private insurers often approve it after prior authorization. The long-term savings from fewer ER visits and hospitalizations often outweigh the drug cost.
Can I stop my heart failure meds if I feel better?
No. Feeling better is a sign the meds are working-not that you’re cured. Stopping them can cause your heart failure to return quickly, sometimes worse than before. Even if your ejection fraction improves, you still need these drugs to protect your heart long-term.
What to Do Next
If you’re on one or two of these meds, ask your doctor: “Am I on all four recommended therapies?” If you’re not, ask why. If cost is the issue, ask about patient assistance programs. If side effects are the problem, ask if switching is possible-like going from ACEI to ARNI, or from furosemide to torsemide.
Heart failure is serious, but it’s not a death sentence. With the right meds, taken correctly, many people live for years with good quality of life. Don’t settle for less than the standard of care. Your heart is worth it.

Josh McEvoy
OMG I switched to Entresto last year and like?? I can actually breathe now 😭 I used to collapse after walking to the fridge and now I’m hiking with my dog 🐶✨ #LifeChanging
January 23, 2026 AT 14:35
Tiffany Wagner
I’ve been on carvedilol for 14 months. At first I felt like a zombie. Now I can play with my grandkids without stopping. Still tired sometimes but worth it. Don’t quit too soon.
January 24, 2026 AT 21:56
Viola Li
Why are we treating heart failure like it’s a puzzle you solve with pills? People used to live with this before Big Pharma invented 4 expensive drugs. Maybe we should fix diets and stress instead of just throwing meds at it.
January 26, 2026 AT 12:47
Jenna Allison
Just want to clarify something real quick - SGLT2 inhibitors like dapagliflozin aren’t just for diabetics anymore. They’re now guideline-recommended for HFrEF AND HFpEF, even if your sugar’s normal. The EMPEROR-Reduced and DAPA-HF trials showed 25-30% reduction in hospitalizations. Also, they’re cheaper than ARNI and often covered by Medicare Part D. Talk to your doc if you’re not on one.
And yes, diuretics can mess with your electrolytes - that’s why I take potassium and magnesium glycinate daily. No more leg cramps at 3 a.m.
Also, if you’re on ARNI, never restart an ACEI without waiting 36 hours. Angioedema isn’t a ‘maybe’ - it’s a hospital emergency. Seen it happen. Not worth it.
And beta blockers? Start low, go slow. I started at 3.125 mg carvedilol twice a day. Felt like I was dying for 2 weeks. Then my energy came back. Now I run 5Ks. It’s a marathon, not a sprint.
Most docs don’t push GDMT hard enough. If you’re only on two meds, ask why. It’s not laziness - it’s systemic. But you can advocate for yourself.
January 28, 2026 AT 09:24
Vatsal Patel
Interesting how we’ve turned medicine into a shopping list. ACEI? Check. ARNI? Check. Beta blocker? Check. Diuretic? Check. But nobody asks why the heart failed in the first place. Is it the sugar? The stress? The 40-hour workweeks? Or just the fact we’re all sitting on couches eating processed crap while our phones tell us we’re ‘doing great’? We treat symptoms like they’re the enemy. The enemy is our lifestyle. Pills don’t fix broken souls.
Also, $550 a month for Entresto? That’s a luxury. Most people in this country can’t afford to be healthy. We’re not treating disease - we’re selling hope at retail prices.
January 28, 2026 AT 23:56
Michael Camilleri
Who even wrote this? Some pharma rep? ARNI is just a fancy combo drug with a fancy name. ACE inhibitors worked fine for decades. Now we’re pushing this expensive thing because the stock prices went up. And don’t get me started on SGLT2 inhibitors - originally for diabetics, now they’re miracle drugs for everyone? Sounds like marketing, not medicine.
My uncle was on lisinopril for 10 years. He lived to 82. No ARNI. No fancy pills. Just walking, no soda, and a low-salt diet. Why are we making this so complicated?
Also, why is everyone on Reddit acting like they’re cardiologists? You take a pill, you feel better, you think you’re an expert. Wake up. You’re not a doctor. Your anecdote doesn’t replace clinical trials.
January 29, 2026 AT 15:06
lorraine england
Just wanted to say thank you for writing this - I’ve been on all four meds for 8 months and I finally feel like myself again. My doctor didn’t push GDMT hard enough at first. I had to research it myself. Now I’m on torsemide instead of furosemide and I sleep through the night. No more 4 a.m. bathroom runs 🙌
Also, if you’re scared of side effects - talk to your pharmacist. They’re way more helpful than you think. And don’t be shy about asking for financial help. There are programs. I got ARNI for $10 a month with a patient assistance card.
You’re not alone. This stuff is hard. But you can do it.
January 30, 2026 AT 07:22
Darren Links
Why do Americans think every problem needs a pill? In my country, we fix things with food, rest, and time. Not 4 different $500/month drugs. This is capitalism disguised as medicine. They’re selling longevity like it’s a subscription service. And now everyone’s addicted to the idea that they need ‘the full quartet’ to survive. What happened to just… living?
Also, I’ve seen 3 people on ARNI with angioedema. One of them almost died. This isn’t science - it’s a gamble with your face.
January 31, 2026 AT 23:55