St. John’s Wort might seem like a harmless way to ease mild depression, but if you’re taking any prescription meds, it could be hiding a serious risk. You’re not alone if you’ve heard it’s a natural alternative to antidepressants - millions take it every year. But here’s the truth most labels won’t tell you: St. John’s Wort can make your blood pressure pills, birth control, antidepressants, or even your transplant meds stop working. And the consequences aren’t theoretical - people have ended up in hospitals, had organ rejections, or gotten pregnant on birth control because of it.
How St. John’s Wort Changes How Your Body Handles Medications
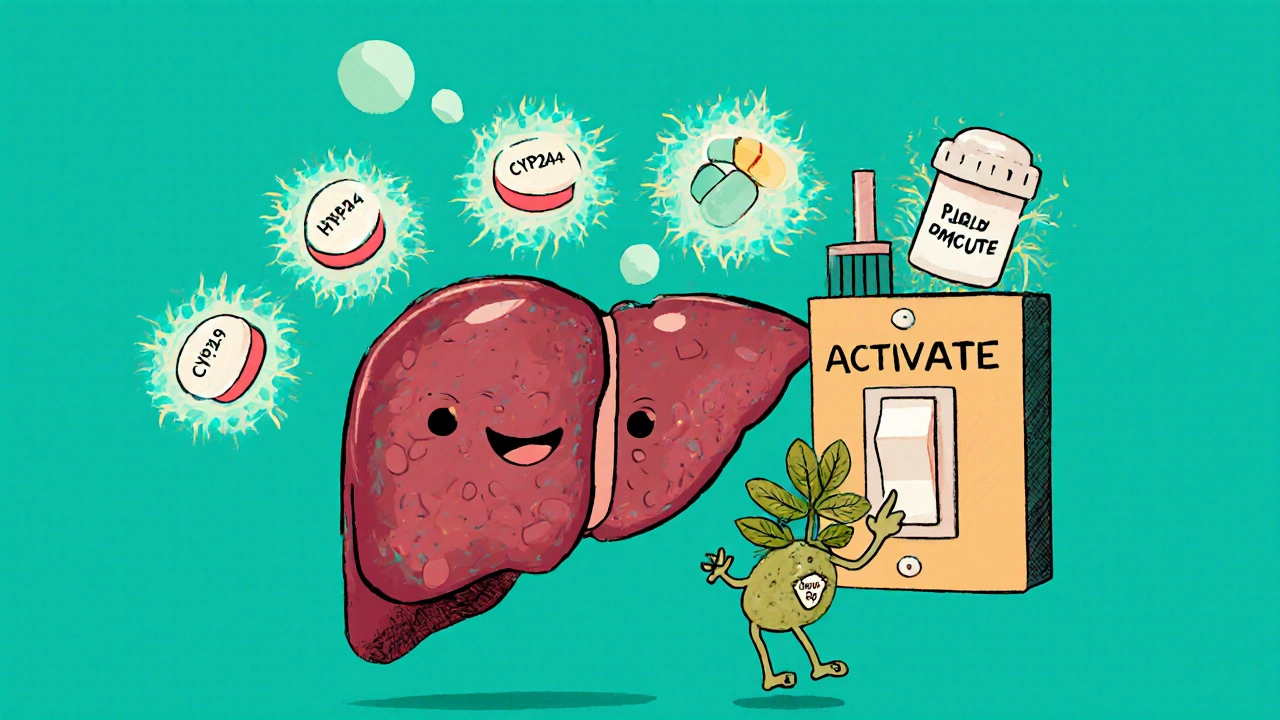
St. John’s Wort doesn’t just sit there. It actively rewires your body’s ability to process drugs. The main culprit is hyperforin, a compound in the plant that turns on a system in your liver called the pregnane-X-receptor, or PXR. When PXR wakes up, it tells your liver to produce more of certain enzymes - especially CYP3A4 and CYP2C9 - that break down medications. It also ramps up P-glycoprotein, a protein that pushes drugs out of your cells before they can do their job.
This isn’t a slow, gentle effect. It starts within days. By day 10, your body is clearing drugs faster than normal. And it doesn’t stop when you quit taking St. John’s Wort - the enzyme surge can stick around for two weeks after you stop. That means even if you take your pill and then switch to St. John’s Wort a week later, your medication may already be losing power.
The Medications That Can Fail Because of It
Over 50 prescription drugs have documented, dangerous interactions with St. John’s Wort. Some of the most critical ones:
- Immunosuppressants like cyclosporine and tacrolimus - used after organ transplants. If levels drop, your body can reject the new organ. There are documented cases of kidney and heart transplant patients rejecting their organs after starting St. John’s Wort, even when they were on the exact same dose they’d been on for months.
- Antiretrovirals for HIV - including protease inhibitors like ritonavir and non-nucleoside reverse transcriptase inhibitors. A drop in drug levels can lead to drug-resistant HIV strains.
- Oral contraceptives - birth control pills, patches, or rings. The FDA has received reports of women getting pregnant while on birth control and taking St. John’s Wort. One woman in a 2019 case report had an unplanned pregnancy after six months of using both.
- Antidepressants - SSRIs like sertraline, SNRIs like venlafaxine, even tricyclics. Combining them with St. John’s Wort can spike serotonin levels too high, leading to serotonin syndrome: agitation, confusion, rapid heart rate, high fever, and in severe cases, seizures or death.
- Anticoagulants like warfarin. One patient’s INR (a measure of blood clotting) dropped from 2.5 to 1.4 in just 10 days after starting St. John’s Wort - putting him at high risk for stroke or clotting.
- Opioids like oxycodone, methadone, and tramadol. St. John’s Wort can reduce their pain-relieving effects, leaving patients in uncontrolled pain.
These aren’t rare edge cases. In Sweden and the UK, regulators forced manufacturers to add bold warnings to both St. John’s Wort and affected prescription labels. In the U.S., the FDA issued a public health advisory in 2000 - but many people still don’t know.
Why People Think It’s Safe - And Why They’re Wrong
St. John’s Wort is sold over the counter. It’s labeled as a “dietary supplement.” That means the FDA doesn’t review it for safety or effectiveness before it hits the shelf. You can buy it in any pharmacy, health store, or online without a prescription. That creates a false sense of security.
People hear “natural,” and they assume “safe.” But natural doesn’t mean harmless. Aspirin comes from willow bark. Digitalis, used for heart failure, comes from foxglove. Nature is full of potent chemicals - and St. John’s Wort is one of the most powerful enzyme inducers known.
Even the packaging can be misleading. Many bottles say “for mood support” or “natural remedy for depression.” Few mention the interaction risks in bold. In Europe, labels must list 12 specific drug classes it interferes with. In the U.S., the warning is often buried in tiny print - if it’s there at all.
Who’s Most at Risk
You’re more likely to be in danger if you:
- Take multiple medications - especially if you’re over 50, managing chronic conditions like high blood pressure, diabetes, or heart disease.
- Have had an organ transplant - even a small drop in immunosuppressant levels can be deadly.
- Are on HIV treatment - losing control of your viral load can have lifelong consequences.
- Use birth control - and want to avoid pregnancy.
- Are trying to manage depression with both prescription meds and herbal supplements.
According to the 2017 National Health Interview Survey, 4.7% of U.S. adults use St. John’s Wort. That number jumps to 8.2% among women aged 35 to 54 - the exact group most likely to be on birth control, antidepressants, or other chronic meds.
What to Do Instead
If you’re considering St. John’s Wort for depression, ask yourself: Are you on any prescription drugs? If the answer is yes - don’t take it. Period.
There are safer alternatives:
- SAM-e - has minimal drug interactions, though it can still raise serotonin levels if combined with SSRIs.
- 5-HTP - also carries some risk with antidepressants, but fewer than St. John’s Wort.
- Cognitive behavioral therapy (CBT) - proven effective for mild to moderate depression, with zero interaction risks.
- Exercise and sunlight - both have strong evidence for improving mood without side effects.
If you’re already taking St. John’s Wort and are on a prescription medication, don’t quit cold turkey. Talk to your pharmacist or doctor. Stopping abruptly can cause withdrawal symptoms - and your body may still be processing the enzyme changes for weeks.

How to Protect Yourself
Here’s what works in real life:
- Always tell your doctor and pharmacist about every supplement you take - even if they don’t ask. Don’t assume they know.
- Use the Drugs.com interaction checker or similar tools before starting anything new. Type in your meds and the supplement. If it says “major interaction,” stop.
- If you’re on a drug with a narrow therapeutic index (like warfarin, cyclosporine, or digoxin), avoid St. John’s Wort entirely.
- Don’t rely on product labels - many U.S. brands still don’t list all risks. Assume it interacts with everything unless proven otherwise.
- If you’re switching from an antidepressant to St. John’s Wort, wait at least two weeks after stopping the prescription to avoid serotonin syndrome.
There’s no safe way to use St. John’s Wort with most prescription drugs. The only exception? If you’re not taking anything else - and even then, you’re still risking unknown side effects or long-term liver impact.
The Bigger Picture
St. John’s Wort sales have dropped 37% since 2000 - not because it stopped working, but because people started dying. Germany still uses it widely for depression, but only after strict doctor supervision. In the U.S., it’s still sold like candy. The European Medicines Agency calls it “unfavorable” for patients on other meds. The American Society of Health-System Pharmacists says its future is shrinking.
Research is exploring low-hyperforin versions that might be safer - but they’re not on shelves yet. Until then, the safest choice is simple: if you’re on a prescription drug, leave St. John’s Wort on the shelf.
Can I take St. John’s Wort with my antidepressant?
No. Combining St. John’s Wort with SSRIs, SNRIs, or other antidepressants can cause serotonin syndrome - a potentially fatal condition marked by high fever, confusion, rapid heartbeat, and muscle rigidity. Even if you feel fine at first, the risk builds over time. If you want to switch from prescription antidepressants to St. John’s Wort, you must do it under medical supervision with a clean break of at least two weeks between stopping one and starting the other.
Does St. John’s Wort make birth control fail?
Yes. St. John’s Wort speeds up the breakdown of estrogen and progestin in birth control pills, patches, and rings. This can cause breakthrough bleeding, reduced effectiveness, and unintended pregnancy. There are documented cases of women getting pregnant while using both. If you’re on hormonal birth control, avoid St. John’s Wort entirely. Use a backup method like condoms if you’ve already taken it.
How long does St. John’s Wort stay in your system?
The herb itself clears from your body in a few days, but its effects on liver enzymes last much longer. It takes about 10 days for enzyme levels to peak, and another two weeks after you stop taking it for them to return to normal. That means if you quit St. John’s Wort today, your medications could still be less effective for up to two weeks. Never assume it’s safe to restart a drug right after stopping the supplement.
Is St. John’s Wort safe after a transplant?
Absolutely not. St. John’s Wort can drop levels of immunosuppressants like cyclosporine and tacrolimus by 30% or more. This has led to organ rejection in multiple documented cases - including heart and kidney transplant patients who were on stable doses for months. There is no safe dose for transplant recipients. Avoid it completely.
Are there any supplements that are safer than St. John’s Wort for depression?
Yes. SAM-e has minimal drug interactions and is effective for mild depression in some studies. 5-HTP is another option, though it still carries some risk with antidepressants. But the safest, most proven approaches are non-supplement: regular exercise, light therapy (especially in winter), and cognitive behavioral therapy. These have no interaction risks and work just as well for mild to moderate depression.
What should I do if I’ve already taken St. John’s Wort with my medication?
Stop taking St. John’s Wort immediately. Contact your doctor or pharmacist. If you’re on a critical drug like warfarin, cyclosporine, or HIV meds, you may need a blood test to check your drug levels. Don’t wait for symptoms. Even if you feel fine, your medication may already be less effective. Going forward, always check for interactions before taking any new supplement - even ones labeled “natural.”


Robert Bashaw
Okay, so let me get this straight - some guy in a lab coat decided that a plant with yellow flowers could outsmart 20 years of pharmaceutical science? And now we’re supposed to believe that St. John’s Wort is just ‘natural’ and ‘harmless’? Nah. This isn’t herbal tea, this is a silent assassin disguised as a wellness trend. I’ve seen people go from ‘I feel better’ to ‘Why is my transplant failing?’ in three weeks. The FDA’s advisory from 2000? Still relevant. Still ignored. Still deadly.
December 1, 2025 AT 07:42
Jennifer Wang
While the post presents a compelling case regarding the pharmacokinetic interactions of Hypericum perforatum, it is imperative to underscore that the induction of CYP3A4 and P-glycoprotein is a well-documented phenomenon in clinical pharmacology. The half-life of enzyme induction is approximately 14 days, as referenced in the British Journal of Clinical Pharmacology (2018). Patients on narrow-therapeutic-index medications, particularly immunosuppressants and antiretrovirals, require mandatory pre-supplement screening. The absence of regulatory oversight in the U.S. dietary supplement industry remains a critical public health gap.
December 3, 2025 AT 03:54
Subhash Singh
Interesting analysis. In India, we have a long tradition of using herbal remedies, but we also have trained Ayurvedic physicians who advise against combining them with allopathic drugs. This article highlights a global blind spot: the assumption that ‘natural’ equals ‘safe.’ I wonder if there are studies comparing the incidence of adverse events in countries where St. John’s Wort is prescription-only versus over-the-counter. Could regulation be the real differentiator?
December 3, 2025 AT 12:15
Sullivan Lauer
Let me tell you something - I used to think St. John’s Wort was my magic bullet. I was depressed after my divorce, I didn’t want to be on SSRIs, I thought, ‘Hey, it’s just a plant!’ So I started taking it. Three weeks later, my anxiety spiked, I couldn’t sleep, and I was sweating like I was running a marathon in July. Turns out, I was on blood pressure meds - and my doctor found my levels had dropped 40%. I almost had a stroke. I’m not exaggerating. I’m not dramatizing. I’m alive because I caught it. Don’t be like me. Don’t wait until your body screams. Just don’t. Stop. Walk away. Your life isn’t worth the risk of a ‘natural’ fix. I’m not mad at you - I’m mad at the system that lets this stuff sit next to gummy vitamins like it’s harmless. It’s not. It’s a grenade with the pin pulled.
December 3, 2025 AT 19:04
Sohini Majumder
ok so like… st. john’s wort? lmao. who even uses this? like, i get it, you’re a 40-year-old woman trying to ‘heal’ your trauma with crystals and chamomile tea, but this? this is just… embarrassing. the fact that people still believe this? 😭. the FDA warned us in 2000 and now we’re still here? i’m not even mad, i’m just… tired. and also, why do these supplements always say ‘for mood support’ like that’s a real medical term? lol. next they’ll sell ‘rainbow unicorn extract’ for diabetes. 🤡
December 4, 2025 AT 22:02
tushar makwana
i come from a small village in india where we use herbs for everything. but we also know when to stop. my grandma always said, ‘if it can change how your medicine works, it’s not a friend - it’s a stranger in your body.’ i read this post and felt it deep. maybe we don’t need more science. maybe we just need to listen to the old ways - the ones that respect both nature and modern medicine. thank you for writing this. i’ll share it with my family.
December 5, 2025 AT 13:23
Richard Thomas
The assertion that St. John’s Wort constitutes a pharmacologically significant inducer of hepatic cytochrome P450 isoforms is empirically substantiated by multiple peer-reviewed studies, including those published in the Journal of Clinical Psychopharmacology and the British Journal of Clinical Pharmacology. The clinical implications for patients on concomitant medications with narrow therapeutic indices - particularly cyclosporine, tacrolimus, and warfarin - are unequivocally severe. The regulatory failure to mandate standardized, legible labeling in the United States represents a systemic dereliction of duty by the FDA and the FTC. This is not a matter of personal choice - it is a public health catastrophe in slow motion.
December 6, 2025 AT 11:11
Monica Lindsey
You’re not ‘natural’ if you’re poisoning people. You’re just irresponsible.
December 7, 2025 AT 16:29
Bernie Terrien
St. John’s Wort is the herbal equivalent of a backdoor exploit in your OS. You think you’re updating your mood - you’re actually giving root access to your liver. And the worst part? The supplement industry knows this. They don’t care. They’re not selling wellness. They’re selling denial. And you’re the product.
December 7, 2025 AT 22:21
stephen idiado
Let’s not conflate correlation with causation. The drop in sales since 2000 correlates with increased awareness, not increased mortality. The cited case reports are anecdotal. Meanwhile, SSRIs have a 30% dropout rate due to side effects. The real issue is pharmaceutical monopolization of mental health narratives. St. John’s Wort is a victim of capitalism, not a villain. Let people choose. Let the market decide.
December 9, 2025 AT 03:46