What Is Aspirin-Exacerbated Respiratory Disease?
Aspirin-Exacerbated Respiratory Disease, or AERD, is not just a bad reaction to painkillers. It’s a chronic, progressive condition that hits adults between 20 and 50, often starting with worsening asthma and persistent nasal congestion. Over time, nasal polyps grow, smell fades, and breathing gets harder-not because of allergies, but because of how the body handles certain drugs. People with AERD react badly to aspirin, ibuprofen, naproxen, and other common NSAIDs. These drugs trigger severe asthma attacks, sinus pressure, and even loss of smell. It’s not an allergy in the traditional sense; it’s a metabolic glitch. When COX-1 is blocked, the body overproduces inflammatory chemicals called cysteinyl leukotrienes, which swell airways and flood sinuses with eosinophils. About 7% of all adult asthmatics have it. Among those with nasal polyps, that number jumps to 14%. Women are slightly more likely to develop it than men.
How Do You Know If You Have AERD?
There’s no single blood test or scan that confirms AERD. Diagnosis relies on three clear signs: asthma, nasal polyps, and respiratory reactions to NSAIDs. If you’ve had asthma since adulthood and suddenly started getting sinus infections or lost your sense of smell after taking ibuprofen, AERD could be the cause. Most patients have had polyps for years before realizing NSAIDs are the trigger. The reactions usually hit within 30 to 120 minutes after taking the drug-think wheezing, nasal congestion, flushing, or even anaphylaxis. If your history is unclear, doctors may recommend a supervised aspirin challenge. This isn’t done in a regular clinic. It happens in a hospital or allergy center with emergency equipment on standby. You’re given tiny, increasing doses of aspirin every 90 to 120 minutes, starting at 20 mg, until you hit 325 mg or react. About 98% of patients who try it under supervision complete the test safely. Blood tests can support the diagnosis: over 75% of AERD patients have high eosinophils (above 500 cells/μL), and nearly 90% show elevated urinary leukotriene E4, a marker of inflammation.
What Happens If You Just Avoid Aspirin and NSAIDs?
Avoiding NSAIDs sounds like the obvious fix. But here’s the catch: stopping aspirin doesn’t stop AERD. The disease keeps progressing. Nasal polyps grow back. Asthma worsens. Smell loss becomes permanent. Studies show that even patients who strictly avoid NSAIDs still need repeat sinus surgeries and steroid bursts. That’s because the inflammation is self-sustaining-it doesn’t need the drug to keep going. Avoidance helps prevent acute reactions, but it doesn’t treat the root problem. That’s why many patients end up stuck in a cycle: take a painkiller → have a reaction → avoid all NSAIDs → polyps return → need surgery → polyps return again. Without targeted treatment, AERD can severely limit daily life. One survey found that 78% of patients reported severe disruption to work, sleep, and social activities due to constant congestion and smell loss.
Medical Treatments: What Actually Works?
First-line treatment focuses on controlling inflammation. High-volume steroid sinus rinses-like 50-100 mg of budesonide mixed in saline, used twice daily-shrink polyps by 30-40% in just eight weeks. Intranasal sprays like fluticasone (two sprays per nostril, twice a day) improve nasal symptoms by 35% on the SNOT-22 scale after 12 weeks. For asthma, medium-dose inhaled steroids combined with long-acting beta agonists (like fluticasone/salmeterol) boost lung function by 15-20% in most patients. If that’s not enough, doctors turn to leukotriene modifiers. Zileuton, which blocks leukotriene production, reduces urinary biomarkers by 75% in two weeks and helps nearly a third of patients report "extreme effectiveness." Montelukast helps too, but only 15% find it highly effective. For the most severe cases, biologics are changing the game. Dupilumab, given as a biweekly shot, cuts polyp size by 55% and improves quality of life scores by 40% in 16 weeks. Mepolizumab, a monthly injection, lowers eosinophils by 85% and reduces the need for future surgeries by 57% over a year.
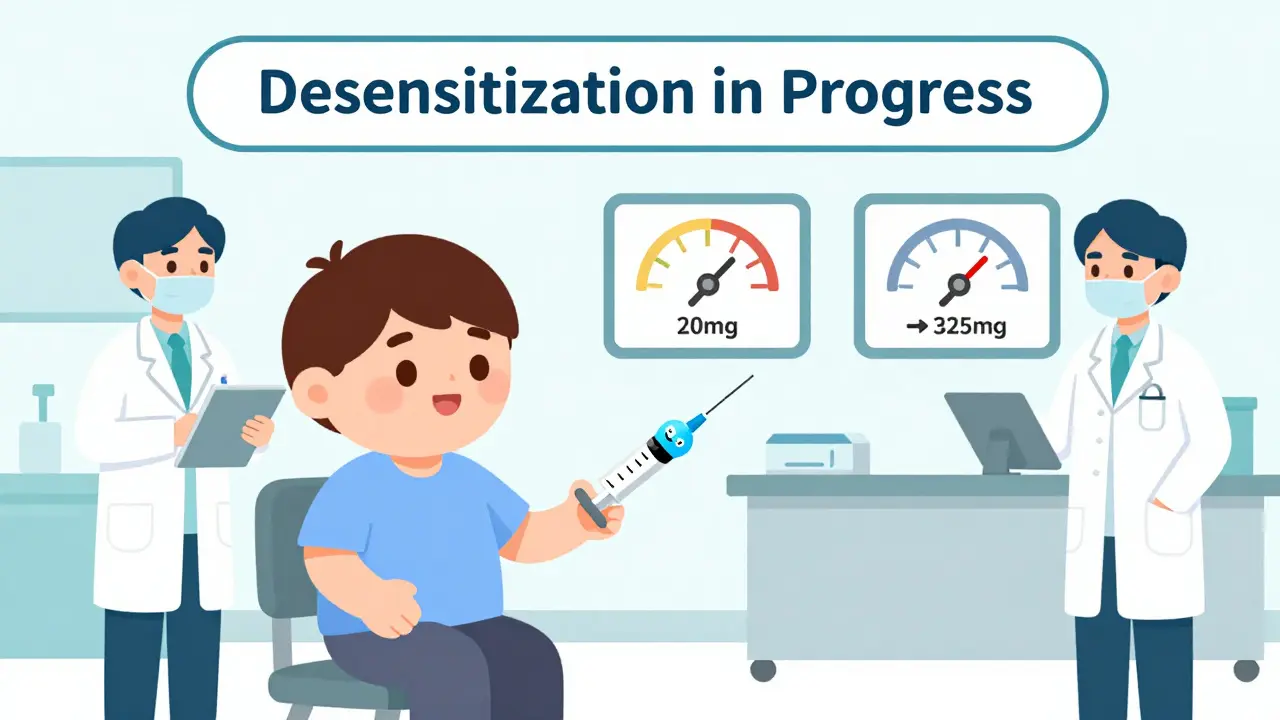
Aspirin Desensitization: The Game-Changer
If you’ve had sinus surgery or are planning it, aspirin desensitization is the most powerful tool you have. It’s not a cure-but it changes the disease’s course. The process takes two days. You start with 20 mg of aspirin, and every 90 to 120 minutes, the dose doubles, climbing to 325 mg. Most patients tolerate it with mild symptoms that resolve quickly. Once you’re desensitized, you take 650 mg of aspirin twice daily, for life. That daily dose keeps inflammation in check. Studies show it slashes the need for oral steroid bursts from 4.2 times a year to just 1.1. It cuts polyp recurrence after surgery from 85% down to 35% over two years. One study found that patients who went through desensitization regained their sense of smell significantly better than those who didn’t-smell test scores jumped from 12.4 to 23.7 out of 40. The American Rhinologic Society and Penn Medicine both call this the gold standard when combined with sinus surgery. But it’s not for everyone. If you have active peptic ulcers, severe heart disease, or can’t commit to daily aspirin, it’s too risky. Missing just two or three doses can undo the effect-68% of patients need to restart the process if they skip doses.
Surgery and the Big Picture
Functional endoscopic sinus surgery (FESS) removes polyps and opens blocked sinuses. Alone, it gives 70-80% of patients relief-but 60-70% get polyps back within 18 months. Add aspirin desensitization, and recurrence drops to 25-30% at two years. Surgeons now recommend doing the surgery first, then starting desensitization a few weeks later. This combo gives the best long-term results. One expert at Brigham and Women’s Hospital put it simply: "Complete sinus surgery followed by aspirin desensitization reduces polyp recurrence by 65% compared to medical therapy alone." But access is a problem. There are only about 35 dedicated AERD centers in the U.S., mostly in big cities. Many patients travel hundreds of miles for the procedure. Telemedicine has helped, but only 18% of U.S. allergists feel confident managing AERD without specialist support.
Real-Life Challenges and Practical Tips
Living with AERD means constant vigilance. Over-the-counter cold meds often contain hidden NSAIDs like ibuprofen or naproxen. Patients on forums like r/SamtersTriad warn about "stealth NSAIDs" in pain relievers, sinus tablets, and even some anti-nausea meds. Many use saline rinses with a drop of tea tree oil to reduce fungal buildup in sinuses. Others take aspirin with food to cut stomach irritation. Cost is another hurdle. Dupilumab and mepolizumab can cost over $30,000 a year, and insurance doesn’t always cover them for AERD. Patients with incomes under $50,000 report that biologics are out of reach. Aspirin desensitization, though, is cost-effective-studies show it saves $12,500 per quality-adjusted life year by preventing repeat surgeries, which average $18,500 each. Over a lifetime, integrated care could save $87,000 per patient in hospital and surgical costs.
What’s Next for AERD Treatment?
The future is promising. New drugs like MN-001 (tipelukast), a dual inhibitor of leukotriene and PDE4, are showing early success in reducing inflammation markers with fewer side effects. Combining dupilumab with aspirin therapy is already proving synergistic-78% of patients on both reach meaningful symptom improvement, compared to 52% on aspirin alone. Regulatory agencies are starting to standardize desensitization protocols, which could expand access. Still, gaps remain. Only 22% of rural AERD patients can reach a specialist within 100 miles. More training is needed for primary care doctors and allergists. But the message is clear: AERD is treatable. It’s not a death sentence. With the right diagnosis and a plan that includes surgery and daily aspirin, most patients regain control of their breathing, their smell, and their lives.
Can you outgrow AERD?
No, AERD is a lifelong condition. It develops in adulthood and doesn’t resolve on its own. While symptoms can be controlled with treatment, stopping management-like skipping daily aspirin-leads to rapid return of inflammation and polyps. There’s no evidence the body ever stops reacting to NSAIDs once AERD is established.
Is it safe to take acetaminophen (Tylenol) if you have AERD?
Yes, acetaminophen is generally safe for people with AERD because it doesn’t strongly inhibit COX-1. Most patients tolerate it well, even at high doses. However, a small subset (about 10-15%) may still react, especially at very high doses or if they have severe disease. Always check with your specialist before using it regularly.
How long does aspirin desensitization take?
The full desensitization process usually takes two consecutive days, with doses given every 90 to 120 minutes. Most patients complete it within 5 to 6 hours per day. After the second day, you’re considered desensitized and can begin daily maintenance dosing. The procedure is done in a controlled setting with medical staff ready to handle any reaction.
What happens if I miss a dose of aspirin after desensitization?
Missing one or two doses is usually okay, but if you skip three or more consecutive days, your body loses tolerance. In 68% of cases, you’ll need to go through the full desensitization process again. That’s why sticking to a daily schedule is critical. Many patients set phone reminders or use pill organizers to stay on track.
Are there any natural remedies for AERD?
No natural remedy has been proven to treat the core inflammation of AERD. Saline rinses, steam inhalation, and humidifiers can help with symptom relief, but they don’t stop polyp growth or leukotriene overproduction. Avoid unproven supplements like butterbur or boswellia-they may interact with medications or worsen inflammation. Stick to evidence-based treatments: steroid rinses, aspirin, and biologics.
What to Do Next
If you suspect you have AERD, start by seeing an allergist or ENT specialist who has experience with the condition. Bring a list of all medications you’ve reacted to, including over-the-counter ones. Ask about getting a nasal endoscopy and a leukotriene E4 test. If you’ve had sinus surgery or are considering it, ask if aspirin desensitization is right for you. Don’t wait until your polyps return again. Early intervention with a comprehensive plan can stop the cycle and restore your quality of life. The tools exist. You just need to find the right specialist to use them.


Conor Murphy
This hit different. I’ve had AERD for 12 years and just found out last year that my constant sinus issues weren’t ‘just allergies’. The smell loss was the worst part. I cried the first time I smelled coffee again after desensitization. 🥲
January 26, 2026 AT 20:31
Paul Taylor
Ive been avoiding NSAIDs for years and thought that was enough but turns out the disease just keeps creeping in like mold in a damp basement polyps come back worse every time and the steroid rinses are a pain but honestly theyre the only thing keeping me breathing
January 26, 2026 AT 21:11
Patrick Merrell
People who just say 'take Tylenol' don't get it. This isn't about painkillers. It's about your body turning on itself. I've seen friends die because they didn't know the difference between a migraine and an AERD flare. No emoji needed. This is life or death.
January 27, 2026 AT 17:46
Conor Flannelly
I used to think AERD was just an Irish thing - lots of us here with chronic sinus issues - but the science says it's global. What's wild is how little the medical system cares. I spent five years getting told I had 'chronic rhinitis' until a grad student at Trinity pointed me to the leukotriene test. The real tragedy isn't the disease - it's how long it takes to get diagnosed. We need more awareness, not just more pills.
January 28, 2026 AT 10:14
Anjula Jyala
If you're not on dupilumab or mepolizumab you're not treating AERD you're just delaying the inevitable. Eosinophil counts above 500 are non negotiable and if your allergist doesn't know what LTE4 is you need a new doctor period
January 28, 2026 AT 23:04
Kirstin Santiago
I just started aspirin desensitization last month and honestly it’s been a game changer. My polyps are shrinking and I can finally sleep without a humidifier. I still use saline rinses with tea tree oil like some people here said - it helps with the fungal gunk. Not magic, but it helps. And yes I set phone alarms for my aspirin. No shame.
January 30, 2026 AT 02:00
Kathy McDaniel
i had no idea this was a thing until my brother got diagnosed and now i look at every medicine label like its a puzzle. i thought ibuprofen was just ibuprofen. turns out its a landmine. i still forget sometimes and get scared but now i know what to do. thanks for this post
January 30, 2026 AT 20:01
April Williams
I can't believe people still think 'natural remedies' help. You're risking your lungs for a tea and a prayer? If you're not on daily aspirin or a biologic after surgery, you're not serious about your health. This isn't yoga. This is science. Stop listening to influencers and get real treatment. Your sinuses will thank you.
January 31, 2026 AT 05:35