Keflex vs Alternatives - Antibiotic Selector
Recommended Antibiotic Options
Quick Takeaways
- Keflex (cephalexin) is a first‑generation cephalosporin ideal for many skin, bone and urinary infections.
- Amoxicillin and penicillin V cover similar Gram‑positive bacteria but differ in resistance patterns.
- Dicloxacillin is better against penicillin‑ase producing Staphylococcus aureus.
- Clindamycin works well for anaerobes and MRSA but carries a higher risk of C. difficile infection.
- Azithromycin and trimethoprim‑sulfamethoxazole (Bactrim) are useful when patients are allergic to beta‑lactams.
What Is Keflex?
Keflex is the brand name for cephalexin, a first‑generation beta‑lactam antibiotic belonging to the cephalosporin class. It was approved in the early 1970s and quickly became a go‑to oral option for uncomplicated skin and soft‑tissue infections, bone infections, and certain urinary tract infections. In Australia, Keflex is classified as a Schedule4 prescription medicine.
Key attributes of cephalexin include:
- Broad activity against Gram‑positive organisms such as Staphylococcus aureus (non‑MRSA) and Streptococcus pyogenes.
- Limited Gram‑negative coverage, mainly Escherichia coli and Proteus mirabilis.
- High oral bioavailability (≈90%); food does not significantly affect absorption.
- Typical adult dose: 250mg to 1g every 6hours, depending on infection severity.
Common Alternatives to Keflex
When a clinician reaches for an alternative, they usually consider the infection type, bacterial resistance, patient allergies, and cost. Below are the most frequently mentioned substitutes.
Amoxicillin is a broad‑spectrum penicillin that treats many of the same infections as Keflex, especially respiratory and ear infections. It is often combined with clavulanic acid to overcome beta‑lactamase resistance.
Dicloxacillin is a penicillinase‑resistant penicillin that targets Staphylococcus aureus strains producing beta‑lactamase, making it a preferred choice for cellulitis when penicillin‑resistance is suspected.
Clindamycin covers many Gram‑positive cocci and anaerobes, and it penetrates bone well, making it useful for osteomyelitis and certain MRSA infections.
Azithromycin is a macrolide with a long half‑life, convenient once‑daily dosing, and activity against atypical pathogens like Mycoplasma. It’s often used when patients cannot tolerate beta‑lactams.
Trimethoprim‑sulfamethoxazole (commonly known as Bactrim) offers good coverage of many urinary pathogens and some skin infections, especially when MRSA is a concern.
Penicillin V remains a classic choice for streptococcal pharyngitis and mild skin infections but lacks activity against beta‑lactamase‑producing staph.
Ciprofloxacin is a fluoroquinolone with strong Gram‑negative coverage, useful for complicated urinary infections but generally avoided for uncomplicated skin infections due to tendon toxicity risks.

Side‑by‑Side Comparison
| Antibiotic | Spectrum | Typical Use | Standard Adult Dose | Common Side Effects | Approx. Cost (AU$) | Pregnancy Category (Australia) |
|---|---|---|---|---|---|---|
| Keflex (Cephalexin) | Gram‑positive + limited Gram‑negative | Skin, bone, uncomplicated UTI | 250mg-1g q6h | Diarrhea, nausea, rash | ~$15 for 30 tablets | B1 |
| Amoxicillin | Broad Gram‑positive + Gram‑negative | Respiratory, ear, dental | 500mg TID or 875mg BID | Diarrhea, hypersensitivity | ~$12 for 30 tablets | B1 |
| Dicloxacillin | Gram‑positive, penicillin‑ase resistant | Cellulitis, abscesses | 500mg QID | GI upset, neutropenia (rare) | ~$20 for 30 tablets | B1 |
| Clindamycin | Gram‑positive + anaerobes | Bone, bite wounds, MRSA (susceptible) | 300mg QID | C. difficile colitis, metallic taste | ~$30 for 30 tablets | B1 |
| Azithromycin | Gram‑positive + atypicals | Respiratory, chlamydia, skin (if beta‑lactam allergic) | 500mg day1, then 250mg daily×4days | GI upset, QT prolongation | ~$25 for 5‑day course | B1 |
| Trimethoprim‑sulfamethoxazole | Gram‑negative + some Gram‑positive, MRSA | UTI, some skin infections | 800mg/160mg BID | Rash, hyperkalemia, renal effects | ~$18 for 30 tablets | C |
| Penicillin V | Gram‑positive (streptococci) | Pharyngitis, mild skin infections | 500mg QID | Allergic reactions, GI upset | ~$10 for 30 tablets | B1 |
| Ciprofloxacin | Broad Gram‑negative, limited Gram‑positive | Complicated UTI, prostatitis | 500mg BID | Tendonitis, QT prolongation | ~$22 for 30 tablets | C |
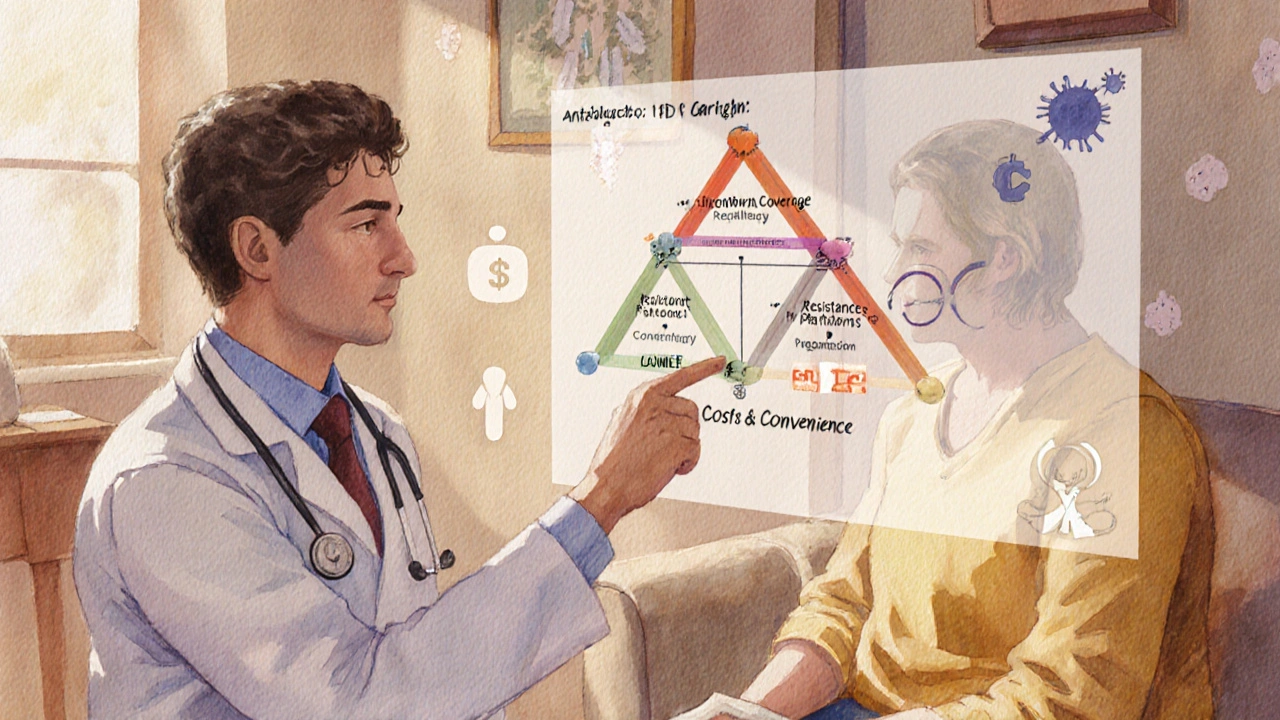
How to Choose the Right Antibiotic
Picking the best drug isn’t a one‑size‑fits‑all decision. Consider these four axes:
- Microbial coverage: Match the antibiotic’s spectrum to the suspected pathogen. For pure staph skin infections, Keflex or Dicloxacillin work well. If MRSA is likely, clindamycin or trimethoprim‑sulfamethoxazole are better bets.
- Patient factors: Allergy history (beta‑lactam allergy pushes you toward azithromycin or clindamycin), renal function (dose‑adjust cephalexin in CKD), pregnancy (avoid CategoryC drugs like Bactrim unless essential).
- Resistance patterns: Check local antibiograms. In many Australian regions, penicillin‑resistant Staph aureus rates are rising, making dicloxacillin or a non‑beta‑lactam option more sensible.
- Cost & convenience: Short courses (azithromycin’s 5‑day regimen) improve adherence, but price spikes can be a barrier for low‑income patients.
For uncomplicated cellulitis in a non‑allergic adult, Keflex remains a cost‑effective first line. If the patient reports a penicillin allergy, azithromycin or clindamycin become viable alternatives.
Safety Profile and Drug Interactions
All antibiotics carry risk. Here are the most relevant for the agents above.
- Keflex: Generally well tolerated; rare severe allergic reactions. Can potentiate warfarin effects - monitor INR if co‑prescribed.
- Amoxicillin: High rates of mild GI upset; p‑aminosalicylic acid in high‑dose combos may cause seizures.
- Dicloxacillin: May cause neutropenia; monitor CBC with prolonged therapy.
- Clindamycin: Strong association with C.difficile colitis - reserve for cases where other options fail.
- Azithromycin: Prolongs QT interval; avoid in patients on other QT‑prolonging meds.
- Trimethoprim‑sulfamethoxazole: Can raise potassium; caution with ACE inhibitors or potassium‑sparing diuretics.
- Ciprofloxacin: Tendon rupture risk, especially in >60years or concurrent steroids.
Availability in Australia (2025)
As of October2025, most of the mentioned antibiotics are listed on the Australian PBS (Pharmaceutical Benefits Scheme) with varying co‑payment thresholds. Keflex is subsidized for a 10‑day supply, costing patients roughly $5 after PBS contribution. Azithromycin’s 5‑day pack is also PBS‑eligible, whereas clindamycin often requires a private script, pushing its out‑of‑pocket price higher.
Bottom Line
If you need a reliable, inexpensive oral antibiotic for routine skin or bone infections and have no beta‑lactam allergy, Keflex alternatives such as amoxicillin or dicloxacillin are excellent back‑ups. When resistance or allergy limits beta‑lactams, shift to clindamycin, azithromycin, or trimethoprim‑sulfamethoxazole depending on the infection site.
Frequently Asked Questions
Can I use Keflex for a urinary tract infection?
Yes, for uncomplicated cystitis caused by susceptible E.coli, a typical adult regimen is 500mg every 6hours for 5‑7days. However, many clinicians now prefer trimethoprim‑sulfamethoxazole or nitrofurantoin because of rising cephalexin resistance.
What should I do if I develop a rash while taking Keflex?
Stop the medication immediately and contact your GP. A rash can signal a mild allergy, but if you notice swelling, breathing difficulty, or widespread hives, seek emergency care as it may be anaphylaxis.
Is it safe to take Keflex with alcohol?
Keflex does not have a direct interaction with alcohol, but drinking heavily can worsen stomach upset and impair immune response, so moderation is advisable.
How long does it take for Keflex to start working?
Because of its high oral bioavailability, blood levels rise within 30‑60minutes. Most patients notice symptom improvement within 2‑3days, although the full course should be completed to prevent relapse.
Can I use Keflex during pregnancy?
Keflex is CategoryB1 in Australia, meaning animal studies show no fetal risk and there are no adequate human studies. It is generally considered safe when benefits outweigh potential risks, but always discuss with your obstetrician.


Michael Leaño
Great overview! I love how the guide lays out the options side‑by‑side, making it easy to spot the right fit for each infection. For someone juggling a mild penicillin allergy, seeing azithromycin and clindamycin front‑and‑center is a real lifesaver. The cost breakdown for Australian patients also helps when budgeting for a full course. Remember to finish the prescribed length even if you feel better after a couple of days – that’s the key to preventing resistance. If you’re ever unsure, a quick chat with your pharmacist can clarify the best choice for your situation.
October 8, 2025 AT 12:14
Anirban Banerjee
In addition to the points raised, it is imperative to align the antibiotic selection with both microbiological data and patient‑specific factors. When an organism is known to produce β‑lactamase, agents such as dicloxacillin or a β‑lactam/β‑lactamase inhibitor combination become preferable. Equally, renal function must be assessed; cephalexin dosage requires adjustment in moderate to severe impairment. For pregnant patients, the categorisation of agents (B1 for cefalexin, C for trimethoprim‑sulfamethoxazole) should guide prescribing decisions. Moreover, local antibiograms provide valuable insight into prevailing resistance trends, thereby refining empirical therapy. Lastly, adherence is enhanced by simplifying regimens – a once‑daily azithromycin course exemplifies this principle. By integrating these considerations, clinicians can optimise outcomes while mitigating adverse effects.
October 9, 2025 AT 02:08
Mansi Mehra
While the table is clear, the cost figures could be updated for 2025.
October 9, 2025 AT 16:01
Jagdish Kumar
Ah, the drama of choosing the perfect antimicrobial! One must not merely glance at a chart but appreciate the nuanced ballet of spectrum, pharmacokinetics, and patient narrative. Imagine a clinician, poised like a maestro, selecting clindamycin for a stubborn MRSA‑laden bite wound, fully aware of the ominous C. difficile shadow. Yet, with a gentle smile, they also recognise the elegance of a short, once‑daily azithromycin regimen for a compliant patient. Such decisions elevate medicine from routine task to an art form, worthy of applause.
October 10, 2025 AT 05:54
Aminat OT
Honestly, I feel kinda left out when people just list drugs without sharing personal stories – I once took Keflex for a nasty skin rash and felt like a hero battling germs, lol. It’s funny how the side‑effects like mild nausea can feel like a betrayal, you know? If u ever wonder whether it’s safe with alcohol, just remember that my friend mixed a couple of beers and felt fine, but that’s not a medical advice. Also, the cost in Australia seems low, but for us in other places it can be a real pain in the wallet. Anyway, stay safe and don’t forget to finish the whole pack, even if you feel better early!
October 10, 2025 AT 19:48
Amanda Turnbo
Let’s be clear: the guide is solid, but it glosses over the ecological impact of broad‑spectrum agents. Using amoxicillin when a narrow‑spectrum cephalexin would suffice contributes unnecessarily to resistance. Likewise, the brief mention of QT prolongation with azithromycin deserves a stronger warning, especially for patients on other cardiotoxic drugs. On the other hand, the inclusion of cost data is commendable and helps patients make informed choices. In practice, I advise clinicians to reserve clindamycin for confirmed MRSA or anaerobic infections, not as a catch‑all alternative. Balancing efficacy, safety, and stewardship remains the ultimate goal.
October 11, 2025 AT 09:41
Jenn Zuccolo
When we contemplate the act of prescribing an antibiotic, we are, in essence, navigating the delicate equilibrium between human health and microbial ecology. Each molecule, from cefalexin to ciprofloxacin, carries with it a narrative that extends beyond the immediate patient to the broader tapestry of bacterial evolution. The guide presents a pragmatic matrix, yet beneath the statistics lies a philosophical question: do we prioritize immediate cure or long‑term stewardship? Consider the case of clindamycin; its potency against anaerobes is undeniable, but the specter of C. difficile looms like an inevitable consequence of hubris. Likewise, azithromycin’s convenient dosing schedule tempts both clinician and patient, yet its propensity to elongate the QT interval reminds us that convenience must never eclipse caution. The cost analysis, while helpful, also invites reflection on the commodification of health-does a lower price point inadvertently promote overuse? In the realm of pregnancy, categorisation B1 for cefalexin offers reassurance, but the lack of robust human data challenges our confidence. Moreover, the practice of adjusting cephalexin dosage for renal insufficiency underscores the necessity of individualized care, a principle that transcends any algorithm. One might argue that the very existence of such guides signals a collective desire to democratise medical knowledge, reducing dependence on opaque specialist jargon. Yet, the reliance on local antibiograms emphasizes that no universal truth exists; each community's microbial landscape paints its own story. In this light, the recommendation to consult a pharmacist becomes not merely a procedural footnote, but a call to interdisciplinary collaboration. Ultimately, the decision matrix is a mirror reflecting our values: we choose between the swift certainty of a broad‑spectrum agent and the disciplined restraint of a narrow‑spectrum alternative. By embracing the nuance presented here, we honour both the patient before us and the unseen microbial world awaiting our choices. The guide, therefore, serves as both a practical tool and a catalyst for deeper contemplation on the ethics of antimicrobial therapy.
October 11, 2025 AT 23:34
Courtney The Explorer
From a strategic standpoint, antimicrobial stewardship is a national security imperative; the misuse of agents like cefalexin directly undermines our healthcare sovereignty-particularly when foreign resistance genes infiltrate domestic microbial reservoirs. This guide's comparative data serves as tactical intel, enabling clinicians to deploy the most cost‑effective, efficacy‑optimized regimen while preserving the integrity of our antibiotic stockpiles. Moreover, the emphasis on PBS subsidies aligns with fiscal policy objectives, ensuring that taxpayer‑funded treatments remain accessible without compromising operational readiness. It is essential to integrate pharmacovigilance metrics into prescribing algorithms, thereby fortifying our defensive posture against emergent multi‑drug‑resistant threats. In sum, informed selection of keflex alternatives is not merely a clinical decision; it is an act of patriotism, safeguarding the nation's health assets against the insidious tide of antimicrobial resistance.
October 12, 2025 AT 13:28
Ashleigh Connell
I appreciate the calm, balanced tone of this guide – it feels like a gentle stroll through a garden of antibiotics, each flower labeled with cost, side‑effects, and ideal uses. Seeing the spectrum columns side by side lets you pick the bloom that best fits your patch, whether that’s the reliable daisy of cefalexin or the exotic orchid of azithromycin. The practical tips about renal dosing and pregnancy categories are like friendly signposts along the path. I also like that the guide acknowledges the emotional side of taking meds, reminding us that finishing the course is a small act of self‑care. Overall, it’s a refreshing read that blends science with a touch of poetic simplicity.
October 13, 2025 AT 03:21
Erin Knight
The comparative table offers a concise snapshot yet omits granular pharmacodynamic parameters that would benefit a rigorous appraisal. For instance, minimum inhibitory concentration (MIC) distributions across prevalent strains are absent, limiting the clinician’s ability to gauge potency beyond generic spectrum descriptors. Additionally, the cost figures, while useful, lack context regarding insurance coverage variability across different states. The discussion of adverse effect profiles could be expanded to include incidence rates, allowing for a more quantitative risk assessment. Nevertheless, the guide succeeds in presenting a user‑friendly layout, which is commendable for a broad audience. In future revisions, integrating antibiogram data and real‑world effectiveness studies would elevate the resource from a superficial overview to a truly evidence‑based decision‑support tool.
October 13, 2025 AT 17:14
Kavita Jadhav
Reading through the guide, it’s clear that each antibiotic has its own story, and matching that story to a patient’s unique circumstances is essential. If you’re dealing with a mild skin infection and have no beta‑lactam allergy, cefalexin remains a solid first choice, offering both efficacy and affordability. However, should an allergy or suspected MRSA be in play, the guide wisely points you toward clindamycin or trimethoprim‑sulfamethoxazole, underscoring safety first. Remember to verify renal function before dosing cefalexin in older adults, as accumulation can lead to unnecessary side‑effects. Finally, never underestimate the power of clear communication: explaining the rationale behind the selected drug fosters adherence and peace of mind. By balancing clinical evidence with compassionate dialogue, you empower patients to engage actively in their own recovery.
October 14, 2025 AT 07:08