When a man starts feeling constantly tired, loses interest in sex, or notices he’s gaining belly fat despite no change in diet, it’s easy to blame stress or aging. But for many, these aren’t just signs of getting older-they’re red flags for male hypogonadism, a condition where the body doesn’t make enough testosterone. It’s more common than most people think: about 1 in 4 men over 60 have testosterone levels below the clinical threshold, and nearly half of those are symptomatic. The problem? Most don’t get tested. And without a proper diagnosis, they’re left guessing why they feel off.
What Exactly Is Male Hypogonadism?
Male hypogonadism means your testes aren’t producing enough testosterone-the hormone that drives muscle growth, bone density, libido, energy, and even mood. It’s not one condition, but two distinct types, each with different causes and treatments.
Primary hypogonadism happens when the testes themselves are damaged or dysfunctional. This could be due to genetic issues like Klinefelter syndrome (an extra X chromosome), past mumps infections that damaged the testicles, or iron overload from hemochromatosis. In these cases, the brain sends strong signals (high LH and FSH hormones) to tell the testes to produce more testosterone-but they just can’t respond.
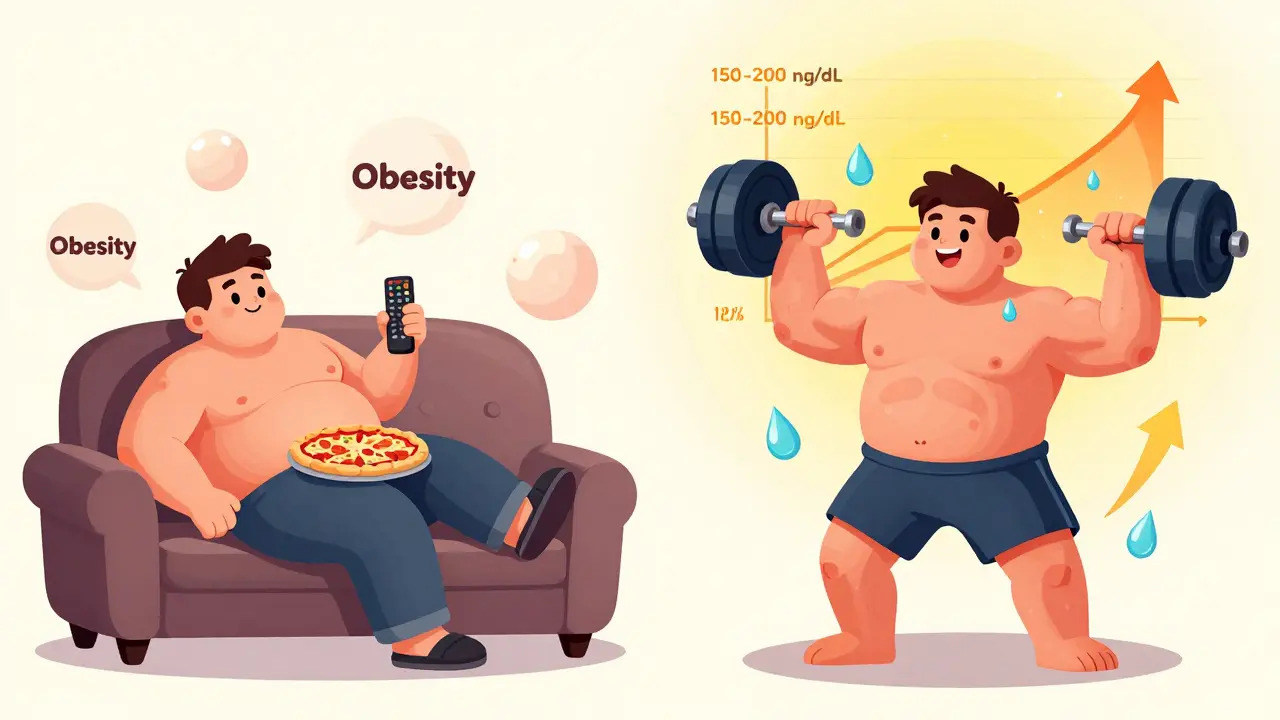
Secondary hypogonadism is far more common, making up 85-90% of cases. Here, the problem isn’t the testes-it’s the brain. The hypothalamus or pituitary gland fails to send the right signals. Obesity is the biggest culprit: men with a BMI over 30 often have 30-50% lower testosterone. Other causes include long-term opioid use, pituitary tumors, or even chronic stress. The good news? Losing just 10% of body weight can boost testosterone by 150-200 ng/dL in many cases.
What Are the Real Symptoms?
Low testosterone doesn’t just mean a low sex drive. It’s a whole-body issue. The most reliable signs include:
- Reduced spontaneous erections-78% of men with confirmed hypogonadism report fewer morning erections
- Loss of libido-85% of diagnosed men say sex no longer interests them
- Testicles smaller than 15 mL (about the size of a walnut)
- Loss of muscle mass-up to 30% reduction over time
- Increased body fat, especially around the abdomen
- Chronic fatigue, even after a full night’s sleep
- Mood changes: irritability, depression, lack of motivation
- Anemia-hemoglobin dropping below 13.5 g/dL
- Bone thinning-33% of untreated men develop osteoporosis
These symptoms don’t show up overnight. They creep in slowly, often mistaken for aging. But here’s the key: if you’re under 50 and experiencing three or more of these, it’s not normal. And if you’re over 60 and suddenly feel worse than you did five years ago, it’s worth checking.
How Is It Diagnosed?
You can’t diagnose low testosterone from symptoms alone. Blood tests are mandatory. But not just any test.
The American Urological Association says a total testosterone level below 300 ng/dL is the clinical cutoff. But that’s not the whole story. Many men with levels between 250-350 ng/dL still feel fine. Others with levels at 320 ng/dL feel terrible. That’s why doctors look at free testosterone-the active, unbound portion. If it’s below 65 pg/mL, treatment is usually recommended, even if total testosterone is borderline.
Testing must be done in the morning-between 8 a.m. and 11 a.m.-because testosterone naturally peaks then. One test isn’t enough. You need two separate morning tests, both below 300 ng/dL, using mass spectrometry. Immunoassays (cheaper, more common tests) can give false highs by 15-20%, leading to misdiagnosis.
Doctors also check LH, FSH, prolactin, and hematocrit. High LH/FSH points to primary hypogonadism. Low or normal levels point to secondary. High prolactin might mean a pituitary tumor. And if your hematocrit is over 50%, you’re at risk for blood clots-this changes treatment options.
Treatment Options: What Actually Works?
Testosterone replacement therapy (TRT) is the standard. But not all methods are equal. Here’s how the main options stack up:
| Method | Dosing | Pros | Cons | Cost (Monthly) |
|---|---|---|---|---|
| Topical Gel | 5-10 g daily | Steady levels, easy to use | Can transfer to partners; skin irritation | $150-$300 |
| Injections (Cypionate/Enanthate) | 100-200 mg every 7-14 days | Low cost, effective | Peaks and crashes; mood swings | $30-$50 |
| Buccal Tablets | 30 mg twice daily | No skin transfer, steady release | Gum irritation, frequent dosing | $200-$400 |
| Subcutaneous Pellets | 150-450 mg every 3-6 months | No daily effort, stable levels | Surgery required; risk of infection | $500-$1,000 per insertion |
| Oral (Jatenzo) | One capsule with high-fat meal | No skin transfer, no injections | Requires meal timing; liver monitoring | $400-$600 |
Most men start with gels or injections because they’re accessible and affordable. Pellets are great for those who hate daily routines but can’t handle frequent doctor visits. Oral testosterone (Jatenzo) is the newest option-it avoids skin contact risks and works well for men who travel or work in close quarters.
Who Shouldn’t Use TRT?
TRT isn’t for everyone. The FDA and Endocrine Society warn against it for men with:
- Prostate cancer (current or past)
- Untreated severe sleep apnea
- Untreated heart failure
- Hematocrit above 50% (risk of clots)
- Uncontrolled polycythemia
There’s also debate around heart health. The FDA added a black box warning in 2015 after studies showed a 30% spike in heart attacks during the first 90 days of TRT in men over 65. But newer research, including the 2022 Testosterone Trials, found no increased risk in men without pre-existing heart disease. In fact, men who stayed on TRT long-term showed a 30% lower death rate than those who didn’t. The key? Proper screening and monitoring.
What About Lifestyle Changes?
If your low testosterone is tied to obesity, TRT isn’t the first step-it’s the last. Losing 10% of your body weight can raise testosterone levels as much as a low-dose injection. Resistance training, especially heavy compound lifts (squats, deadlifts), boosts natural production. Sleep matters too: men who sleep less than 5 hours a night have 15-20% lower testosterone.
One study from UCSF followed 500 men with obesity-related hypogonadism. After 18 months, 65% of those who lost 10% of their body weight stopped TRT entirely. Only 12% of men with genetic causes (like Klinefelter) could stop. That’s the difference between a fixable problem and a lifelong condition.

What Happens After You Start?
TRT isn’t a set-it-and-forget-it treatment. You need follow-up:
- Check hematocrit every 3-6 months (keep it under 50%)
- Test PSA at baseline and again at 3-6 months
- Monitor symptoms with the Aging Males’ Symptoms (AMS) scale
- Re-test testosterone levels at 3 months to adjust dose
Side effects are common but manageable. Acne? Use non-comedogenic cleansers. Mood swings from injections? Switch to gels or pellets. Testicular shrinkage? That’s normal-TRT suppresses natural production. If you want to preserve fertility, you’ll need hCG or clomiphene alongside TRT.
And here’s something most don’t tell you: 30% of men on TRT feel no improvement-even with perfect testosterone levels. Why? Because their fatigue, low mood, or brain fog might be caused by sleep apnea, thyroid issues, or depression. TRT fixes low testosterone-not everything.
What’s Next in Treatment?
The future of hypogonadism treatment is personalization. Researchers are moving away from the “one size fits all” approach. Instead, they’re looking at phenotypes: Is your issue mostly about muscle loss? Mood? Sexual function? Bone density? Each response may need a different blend of therapy.
Emerging drugs like SARMs (selective androgen receptor modulators) show promise. Unlike testosterone, they don’t shut down natural production or raise red blood cell counts. Enobosarm, in Phase III trials, increased muscle mass by 70% without suppressing LH or FSH. But they’re not FDA-approved yet.
The TRAVERSE trial, tracking 5,000 men over five years, will give us the clearest picture yet on whether TRT increases heart risk. Results are due in 2025. Until then, the safest approach is this: treat only those with clear symptoms and confirmed low levels-not just because you want to feel younger.
Final Thoughts
Male hypogonadism is treatable. But it’s not a quick fix. It’s a medical condition that requires diagnosis, monitoring, and patience. If you’re tired, unmotivated, and losing muscle, don’t just accept it as aging. Get tested. Rule out other causes. And if it’s low testosterone, know that effective, safe treatment exists.
But don’t chase testosterone like a magic pill. It’s a tool-not a cure-all. The best results come from combining treatment with weight loss, strength training, and good sleep. That’s how you get your energy back, your body back, and your life back.
Can low testosterone cause depression?
Yes. Low testosterone is strongly linked to low mood, lack of motivation, and irritability. In clinical studies, about 60% of men with confirmed hypogonadism report depressive symptoms. TRT often improves mood within 4-8 weeks, but if depression persists, it’s important to rule out other causes like thyroid problems or sleep disorders.
Is testosterone therapy safe for older men?
For men over 65 with no history of heart disease or prostate cancer, TRT is generally safe when properly monitored. The biggest risk is polycythemia-thickened blood-which can be managed with regular blood tests and phlebotomy if needed. The FDA’s black box warning applies mainly to men with existing cardiovascular disease or those starting TRT without proper screening.
Can I get testosterone without a prescription?
No. In Australia and the U.S., testosterone is a controlled substance. Buying it online or from unregulated sources is illegal and dangerous. Products sold as “natural testosterone boosters” rarely raise levels significantly and may contain hidden steroids. Always get tested and prescribed by a licensed doctor.
Will TRT make me grow more hair or cause baldness?
Testosterone itself doesn’t cause baldness. Hair loss is driven by genetics and the enzyme 5-alpha-reductase, which converts testosterone to DHT. If you’re genetically prone to male pattern baldness, TRT may speed up hair thinning. But it won’t cause baldness in someone who wouldn’t have lost hair anyway. Minoxidil or finasteride can help manage this side effect if needed.
How long does it take to feel better on TRT?
Energy and mood often improve within 2-4 weeks. Libido and erections usually get better by week 6. Muscle mass and strength take longer-most men see noticeable gains after 3-6 months, especially with resistance training. Bone density improvements take 12-24 months. Patience is key.
Can I stop TRT once I start?
You can, but your testosterone levels will drop back to pre-treatment levels. If your hypogonadism is due to obesity or lifestyle, you might be able to stop after weight loss. But if it’s genetic or due to pituitary damage, stopping means symptoms return. Some men use hCG or clomiphene to preserve natural production while on TRT, but this requires careful medical supervision.



Cameron Hoover
Man, I was convinced I was just getting old until I read this. Started getting tested after my wife pushed me - turns out my T was at 240. Started gels, lost 25 lbs, and now I’m lifting again. Feels like I got my 30s back. Don’t ignore the signs.
Also, sleep matters. I started sleeping 7+ hours and noticed the mood shift before the energy did. Crazy how much your brain needs rest.
December 22, 2025 AT 11:15
Stacey Smith
This is why America is falling apart. Men are too lazy to lift weights or lose weight so they want a pill. TRT isn’t a magic fix. Get off the couch. Eat real food. Sleep. Stop blaming your hormones for your laziness.
December 23, 2025 AT 20:10
Ben Warren
While the article presents a clinically informed overview, it is critically deficient in its failure to emphasize the potential for iatrogenic harm associated with testosterone replacement therapy, particularly in the context of erythrocytosis, cardiovascular risk stratification, and the suppression of endogenous gonadotropin secretion. The normalization of biochemical markers without concurrent assessment of functional outcomes - such as quality-of-life metrics, cognitive performance, and metabolic homeostasis - constitutes a significant epistemological flaw in contemporary clinical practice. Moreover, the normalization of TRT as a lifestyle intervention for men under 50, absent definitive evidence of symptomatic hypogonadism, represents a dangerous medicalization of aging.
Furthermore, the omission of long-term data regarding prostate cancer progression under TRT, despite the existence of multiple cohort studies suggesting potential acceleration in high-risk phenotypes, reflects a troubling disregard for precautionary principle in endocrinology. The suggestion that weight loss alone may suffice for obese patients is statistically valid but clinically naive; the vast majority of such patients fail to sustain weight loss beyond 12 months, rendering the intervention functionally irrelevant in real-world settings.
December 24, 2025 AT 16:42
Teya Derksen Friesen
I’ve seen this happen to so many men in my practice - they come in exhausted, depressed, and blame themselves. But it’s not weakness. It’s biology. The fact that we still treat low T like a taboo is why so many suffer in silence. I wish more doctors would screen proactively instead of waiting for men to ‘hit rock bottom.’
Also, the pellet option? Life-changing for busy professionals. No daily gels, no injections. Just one tiny procedure twice a year. And yes, it’s expensive - but so is losing your job because you can’t focus.
December 26, 2025 AT 12:09
Sandy Crux
Interesting… but where are the citations? You mention ‘a study from UCSF’ - which one? 2017? 2020? And ‘30% of men feel no improvement’ - with what sample size? What was the control group? You’re presenting anecdotal generalizations as if they’re peer-reviewed consensus. Also, why is Jatenzo listed as ‘newest’ when it’s been on the market since 2021? And why no mention of aromatase inhibitors for men with high estrogen conversion? This reads like a pharmaceutical brochure disguised as medical advice.
December 27, 2025 AT 01:02
Hannah Taylor
so like… is this just a big scam? i heard testosterone is used by the gov to control men. like they pump it into the water or something. also my cousin took it and started yelling at his dog. now he’s on 3 meds. i think this is all a lie. also why is it so expensive? i can get ‘natural boosters’ on amazon for 10 bucks. they work better. trust me.
December 27, 2025 AT 20:02
mukesh matav
Thank you for sharing this. In my culture, men don’t talk about this. We just suffer silently. But reading this made me realize it’s not weakness - it’s a medical condition. I’m going to ask my doctor for a test next week. I’ve been tired for years. I thought it was just work.
December 28, 2025 AT 07:43
Peggy Adams
My husband went on TRT and turned into a monster. Started cheating, got aggressive, lost weight like a beast - then said he didn’t need me anymore. So yeah, I’m not buying the ‘it’s just hormones’ line. This stuff changes your personality. And no one warns you.
December 28, 2025 AT 12:48
Sarah Williams
Thank you for writing this. I’ve been pushing my husband to get tested for years. He finally did - and now he’s sleeping through the night, laughing again, and even asked me to go hiking. It’s not a magic pill. But it’s a lifeline. Don’t wait until you’re broken to ask for help.
December 29, 2025 AT 13:51
Dan Adkins
It is imperative to recognize that the prevalence of hypogonadism in sub-Saharan African populations remains grossly underreported due to systemic deficiencies in diagnostic infrastructure. The data cited herein, derived almost exclusively from Western cohorts, cannot be extrapolated to non-Western demographics without acknowledging confounding variables such as nutritional status, parasitic load, and genetic polymorphisms in androgen receptor sensitivity. Furthermore, the normalization of TRT as a universal intervention disregards the potential for endocrine disruption in populations with historically lower baseline testosterone levels. The global applicability of these recommendations is, therefore, scientifically untenable.
December 29, 2025 AT 14:45
Grace Rehman
So we’ve turned men’s bodies into a DIY biohacking project. You’re not aging - you’re just failing to optimize. You’re not tired - you’re low on HGH. You’re not sad - your testosterone is ‘suboptimal.’ We’ve reduced the human experience to a spreadsheet of hormone levels and pellet insertions. What happened to just… being? To accepting that life gets harder? That some days you just feel flat, and that’s okay? Maybe we don’t need more hormones. Maybe we need less pressure to be someone else’s version of ‘strong.’
December 30, 2025 AT 20:47