Medication Side Effect Checker
Check Your Medications
Identify potential side effects and dangerous interactions before your next doctor appointment
When you start a new medication, you’re not just getting a pill-you’re getting a potential chain reaction in your body. Some side effects are mild, like a dry mouth or a little dizziness. Others can be serious enough to land you in the hospital. The good news? You don’t have to guess what’s normal or what’s dangerous. Asking the right questions at your appointment can cut your risk of a preventable adverse reaction by more than 20%.
Why am I taking this medicine?
This is the first question you should ask, even if it feels obvious. Many people take medications for years without knowing why they were prescribed in the first place. A 2023 Cochrane Review found that 15.2% of medications in older adults are continued long after they’re needed. That’s not just waste-it’s risk. Maybe you were put on a blood pressure pill after a hospital stay, but your numbers are now normal. Maybe your doctor prescribed an anticholinergic for sleep, but you’re now experiencing confusion or constipation. If you don’t know the purpose, you can’t judge if the benefits still outweigh the side effects. Ask for a clear, plain-language explanation: “What condition is this meant to treat, and how will I know it’s working?”What are the side effects?
Not all side effects are created equal. Some are common and harmless. Others are rare but dangerous. The National Prescribing Service (NPS) Australia recommends asking specifically about anticholinergic side effects if you’re over 65-these include dry mouth, blurred vision, constipation, urinary retention, and memory issues. These affect 27 bodily systems and are linked to a higher risk of falls and cognitive decline. The Anticholinergic Cognitive Burden Scale (ACB) rates medications on how likely they are to cause these effects. Ask your doctor: “Which side effects are most common? Which ones mean I should call you right away?” Don’t just accept a list from the pamphlet. Get personalized info. For example, if you have glaucoma, certain antidepressants could worsen it. If you have kidney problems, some painkillers could be risky.What can I do about side effects?
This is where most people stop asking-and where the real help begins. Side effects aren’t always something you just have to live with. For example, if metformin gives you stomach cramps, taking it with food reduces gastrointestinal issues in 70% of users. If you’re on a statin and getting muscle aches, switching to a different statin or lowering the dose often helps. Dry mouth from antihistamines? Sipping water, chewing sugar-free gum, or using a saliva substitute can make a big difference. A 2024 Kaiser Permanente study showed patients who asked this question had 22.8% fewer emergency room visits. Write down the side effects you’re experiencing, how often they happen, and what makes them better or worse. Bring that list to your appointment. Your doctor can’t fix what they don’t know you’re dealing with.Are there alternatives?
There’s often more than one way to treat a condition. The Beers Criteria, updated annually by the American Geriatrics Society, lists 56 medications that are potentially inappropriate for older adults because of their side effect profiles. Maybe your doctor prescribed an older antidepressant with strong anticholinergic effects, but there’s a newer one with fewer cognitive risks. Maybe you’re on a daily NSAID for arthritis pain, but acetaminophen or physical therapy could be safer long-term. Ask: “Is there another option with fewer side effects? What are the trade-offs?” Don’t assume the first prescription is the only option. Generic drugs are just as effective as brand names and cost up to 89% less, according to FDA data. Ask if a generic version is available-and if it’s right for you.Do I still need to take this medicine?
Medications aren’t forever. Many people keep taking pills long after the original reason is gone. Blood pressure meds after a single high reading? Anticoagulants after a one-time blood clot? Sleep aids used for months? A 2022 JAMA Internal Medicine study showed that patients who asked about stopping medications were more likely to safely deprescribe and had fewer side effects. Ask: “Can this be stopped? Should I try going off it? How do I do that safely?” Never stop cold turkey-some medications cause dangerous withdrawal. But with proper guidance, many people can reduce or eliminate pills they no longer need.What constitutes a serious side effect?
Not every weird feeling means an emergency. But you need to know the red flags. The FDA defines serious side effects as those that result in death, hospitalization, disability, birth defects, or life-threatening conditions. That’s not vague-it’s specific. If you’re on blood thinners and notice unexplained bruising, nosebleeds, or dark stools, that’s a red flag. If you’re on an antibiotic and develop a rash with blistering or peeling skin, that’s a medical emergency. If you’re on an SSRI and suddenly feel suicidal or have racing thoughts, call your doctor immediately. Don’t wait until your next appointment. Keep a list of these red flags handy. The FDA’s Adverse Event Reporting System shows that 4.2% of reported side effects lead to hospitalization-many of which could have been avoided with earlier detection.Could this interact with other drugs or supplements?
Most people don’t realize that over-the-counter meds, herbal supplements, and even grapefruit juice can change how your prescription works. A 2022 NEJM study found that combining ibuprofen with blood thinners increases bleeding risk by 2.8 times. Diphenhydramine (found in many sleep aids and allergy pills) interacts dangerously with anticholinergics, raising the risk of confusion and falls. If you take five or more medications-which 41.9% of people over 80 do, according to CDC data-the chance of a bad interaction skyrockets. Bring a complete list of everything you take: pills, vitamins, CBD, turmeric, melatonin, even herbal teas. Ask: “Could any of these interfere with my new medicine?” Pharmacists are trained to catch these interactions. Ask them during your refill.Should I take this with food or on an empty stomach?
It sounds simple, but food changes how your body absorbs medicine. Some drugs need food to reduce stomach upset. Others must be taken on an empty stomach or they won’t work. For example, taking certain antibiotics with dairy can block absorption. Taking thyroid medication with coffee or calcium supplements can make it ineffective. The FDA says food interactions affect 40% of medications. Ask: “Does this need to be taken with food, or should I wait an hour before or after eating?” If you’re unsure, check the label or ask your pharmacist. A 2023 Medscape report found that 12.4% of patients can’t even correctly identify their own medications-don’t let confusion over when to take them add to the risk.Will this medicine make any of my other conditions worse?
If you have diabetes, heart disease, kidney problems, or depression, a new medication could make those worse. For example, beta-blockers for high blood pressure can mask low blood sugar symptoms in diabetics. NSAIDs can raise blood pressure and hurt kidney function. Antidepressants can worsen glaucoma or urinary retention. A 2024 Kaiser Permanente study tracked 3.2 million patients and found that asking this single question prevented 1,842 flare-ups of chronic conditions. Don’t assume your doctor knows all your conditions. List them. Say: “I have [condition]. Could this medicine make it harder to manage?”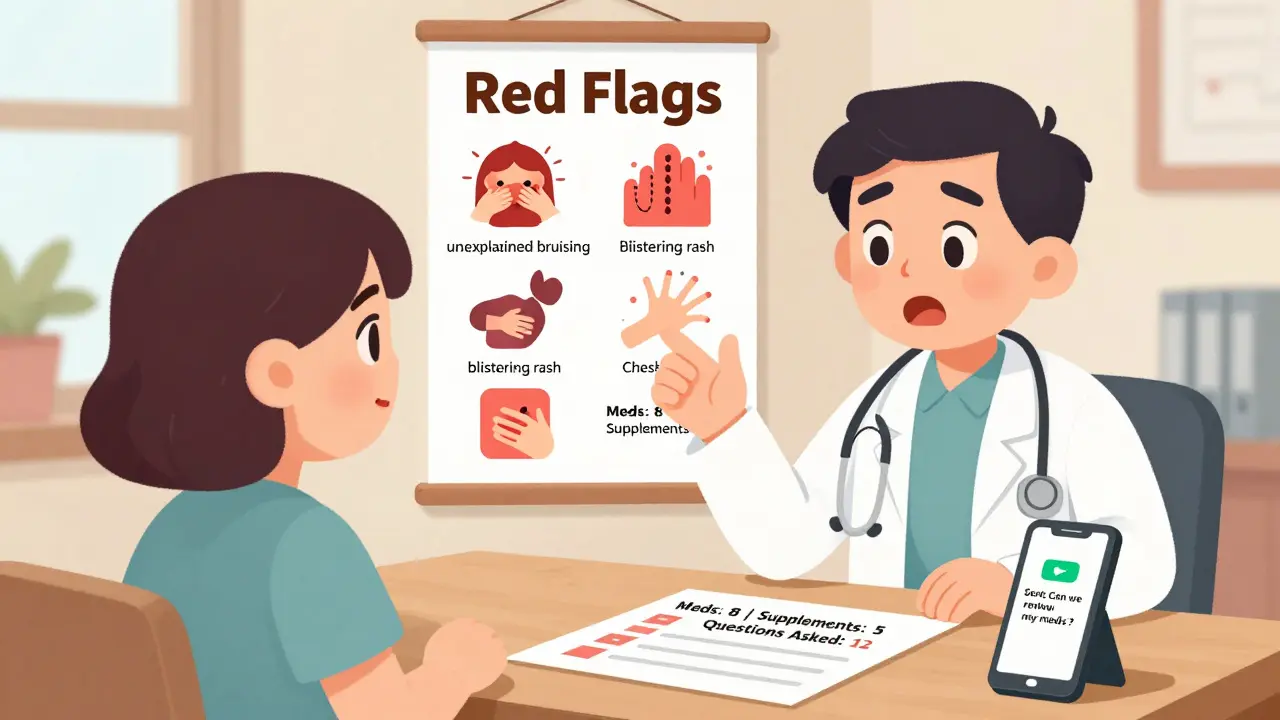
How do I take this correctly?
Medication errors are one of the leading causes of preventable harm. The Institute for Safe Medication Practices (ISMP) says 32.7% of errors happen because patients take the wrong dose, at the wrong time, or in the wrong way. Is it once a day or twice? Morning or night? Should you swallow it whole or split it? Can you crush it? Does it need refrigeration? If you’re using an inhaler, insulin pen, or eye drops, ask for a demonstration. Don’t just nod along. Say: “Can you show me how to use this?” Many clinics now offer video guides or QR codes that link to instructions. If you’re unsure, call your pharmacy. They’re required to answer these questions.When should I call you or go to the ER?
You need a clear action plan. Don’t wait until you’re panicked. Ask: “If I feel [specific symptom], should I call you, go to urgent care, or head to the ER?” Write it down. For example: “If I have chest pain, shortness of breath, or swelling in my legs, call immediately.” “If I get a mild rash, call within 24 hours.” “If I feel dizzy, sit down and wait 10 minutes-if it doesn’t pass, call.” Having this plan reduces anxiety and speeds up care. A 2023 Johns Hopkins study found that patients with written instructions were 41% less likely to delay seeking help.How do I keep track of all this?
Memory fails. Especially when you’re on multiple meds. The Joint Commission says 43.2% of medication errors happen during care transitions-like after a hospital stay or when your doctor changes your prescription. Keep an updated list. Include the name, dose, why you take it, and when. Use your phone, a notebook, or a free app like Medisafe. Update it within 48 hours of any change. Bring it to every appointment. Your pharmacist can help you organize it. A 2023 American Journal of Health-System Pharmacy survey found patients who used a written list had 62% fewer medication errors.What if my doctor dismisses my concerns?
It happens. A 2024 Medscape survey found that 41.3% of patients felt their side effect concerns were ignored-especially with antidepressants, where sexual dysfunction affects up to 73% of users but is only discussed in 52.6% of cases. If your doctor brushes you off, say: “I’m worried this side effect is affecting my quality of life. Can we review my options?” If that doesn’t work, ask for a referral to a pharmacist or a second opinion. Your health isn’t negotiable. You have the right to be heard.What if I forget to ask these questions during my appointment?
Write your questions down before the appointment. Bring them with you. If you run out of time, ask if you can call the office later or schedule a quick follow-up. Many clinics now offer secure messaging through patient portals-use it. You can also ask your pharmacist during your refill-they’re trained to answer medication questions and often have more time than your doctor.
Can side effects show up weeks after starting a medication?
Yes. Some side effects appear days, weeks, or even months later. For example, statins can cause muscle damage after months of use. Antidepressants can trigger suicidal thoughts in the first few weeks. Blood thinners can cause internal bleeding slowly over time. Don’t assume if you felt fine at first, you’re safe. Keep monitoring your body and report new symptoms-even if they seem minor.
Is it safe to stop a medication if I think it’s causing side effects?
Never stop a prescription medication without talking to your doctor. Some drugs, like antidepressants, blood pressure meds, or seizure medications, can cause dangerous withdrawal symptoms if stopped suddenly. Instead, call your doctor and say: “I think this medicine might be causing [symptom]. Can we talk about whether it’s safe to adjust or stop it?”
Do I need to tell my doctor about supplements and herbal remedies?
Absolutely. Supplements like St. John’s Wort, garlic, ginkgo, or fish oil can interact with prescription drugs. St. John’s Wort can make birth control, antidepressants, and blood thinners less effective. Garlic and ginkgo can increase bleeding risk when taken with aspirin or warfarin. Always list everything you take-even if you think it’s “natural” or “harmless.”
How do I know if a side effect is from the medicine or just aging?
It’s not always easy. But if a symptom started after you began a new medication, it’s likely related-even if you’re over 65. Common aging symptoms like memory lapses, fatigue, or dizziness can be worsened or caused by drugs. Ask your doctor: “Could this be related to my medication?” and request a review of your full list. The Beers Criteria exists specifically to help doctors distinguish between aging and medication-induced problems.
If you’re on multiple medications, take a moment right now to write down the names, doses, and reasons for each one. Then, pick one question from this list and ask your next doctor. It’s the simplest, most powerful thing you can do to protect your health.



Simran Kaur
I took my grandma to her appointment last week and wrote down all these questions on a sticky note. She was nervous, but when she asked about stopping her blood pressure med, the doctor actually paused and said, 'You know what? You’re right.' We cut one pill that day. She’s been sleeping better and not dizzy anymore. I cried in the parking lot. This list saved her.
Thank you for writing this.
PS: Bring snacks to the appointment. Hungry patients are cranky patients.
January 27, 2026 AT 10:32
Neil Thorogood
So let me get this straight - you’re telling me I should ask my doctor if I can stop taking a pill they gave me 7 years ago... and they might say YES???
Bro. That’s not medicine. That’s a magic trick.
Also, I took 3 pills today and still don’t know why. 😅💊
January 28, 2026 AT 17:27
Jessica Knuteson
Medication is just another form of control. The system gives you a pill to make you compliant. The real question isn’t what the drug does - it’s why you were ever made to believe you needed it in the first place.
Side effects are just the body screaming. You’re not supposed to hear it.
Ask questions. Still won’t change anything.
January 29, 2026 AT 07:59
shivam utkresth
Yo, this is the most useful post I’ve read since I stopped believing in 'miracle detox teas'.
My uncle was on 11 meds, including melatonin + St. John’s Wort + ibuprofen + a beta-blocker. He thought he was ‘just being healthy.’ Turns out his brain was in a chemical warzone. We got him down to 3. Now he remembers his own birthday. 🙌
Also, never trust a doctor who says ‘it’s fine’ without looking at your list. They’re not gods. They’re humans who forgot their coffee.
January 29, 2026 AT 08:30
rasna saha
As someone from India where people often take antibiotics ‘just in case’ or herbal mixtures from the corner shop - this is gold. My mom still thinks turmeric cures everything. I printed this out and gave it to her with chai. She cried. Then she asked me to help her make a list.
Thank you. This matters so much.
January 30, 2026 AT 08:32
John Wippler
This isn’t just advice - it’s a revolution. We’ve been trained to be passive recipients of pills, not active participants in our own healing. You’re not a patient. You’re a co-pilot.
And if your doctor treats you like a vending machine? Find a new one.
Write your questions. Bring your list. Speak up. Your life isn’t a script. It’s yours to rewrite.
Start today. One question. One pill. One breath.
You got this.
January 30, 2026 AT 11:32
Kipper Pickens
Pharmacokinetic variability across age cohorts, particularly in polypharmacy scenarios, necessitates a dynamic risk-benefit reassessment protocol. The Beers Criteria and ACB scale provide validated frameworks for deprescribing, yet implementation remains suboptimal due to cognitive load and provider time constraints. Patient-initiated inquiry mitigates systemic inertia. Efficacy data from Kaiser and Cochrane confirm statistically significant reduction in AE-related hospitalizations when structured questioning protocols are employed. Recommend integration into EHR prompts.
February 1, 2026 AT 03:48
Aurelie L.
I asked about my antidepressant. Doctor said ‘it’s fine.’ I cried. Then I asked again. He sighed. Then he changed it. So yeah. Ask. Even if it’s hard.
February 1, 2026 AT 20:40
Joanna Domżalska
Why are we even asking doctors? They’re just middlemen for Big Pharma. You want to know side effects? Read the FDA’s adverse event reports. Not what your doctor tells you. What the system hides.
Also, ‘ask questions’? Cute. You think your 8-minute visit is going to change anything?
February 3, 2026 AT 15:37
Faisal Mohamed
Bro, I took my dad to his appointment after he started feeling ‘off’ on his new statin. He had zero muscle pain at first. Then after 3 months - boom. Weakness. Falls. We asked the question about alternatives. Switched to ezetimibe. He’s hiking again. 🙏
Also, grapefruit juice? Don’t. I learned that the hard way. 😅
February 5, 2026 AT 04:17
Josh josh
my doc gave me 5 pills and said ‘take one in the morning’ i asked which one he just shrugged. i still dont know. this post saved me. thanks.
February 6, 2026 AT 05:44
Robin Van Emous
I’ve been a nurse for 22 years. I’ve seen patients get hurt because they didn’t ask. I’ve seen doctors miss things because they assumed. This list? It’s not just helpful - it’s necessary.
Bring your list. Write down your symptoms. Say, ‘I’m scared.’
And if your doctor gets annoyed? That’s not your problem. That’s theirs.
You’re not being difficult. You’re being smart.
And you deserve to be heard.
Go do it.
February 7, 2026 AT 09:30